The Paitent Reported Measures Program (PRMs) is guided by the following principles:
- Patient-centred: Designed to give patients a stronger voice in their care.
- Co-designed: Developed with input from patients, carers, clinicians and decision makers.
- Integrated: Applied across all care settings to provide a complete view of the patient journey.
- Fit-for-purpose and meaningful: Relevant and useful for diverse users, including patients, carers, clinicians and decision makers.
- Trusted and reputable: Evidence-based, culturally appropriate and easy to understand.
- Consistent: Enables comparison across care dimensions while allowing local flexibility.
- Universal coverage: Broadly applicable, with the ability to distinguish between different patient cohorts.
- Sustainable: Supports long-term, efficient and effective healthcare delivery.
- Transparent: Provides real-time data access across all levels of the health system.
- Staged implementation approach: Allows for gradual adoption with appropriate change management and support.
Governance structure
The PRMs program is supported by a structured governance model that ensures alignment with strategic goals and effective implementation.
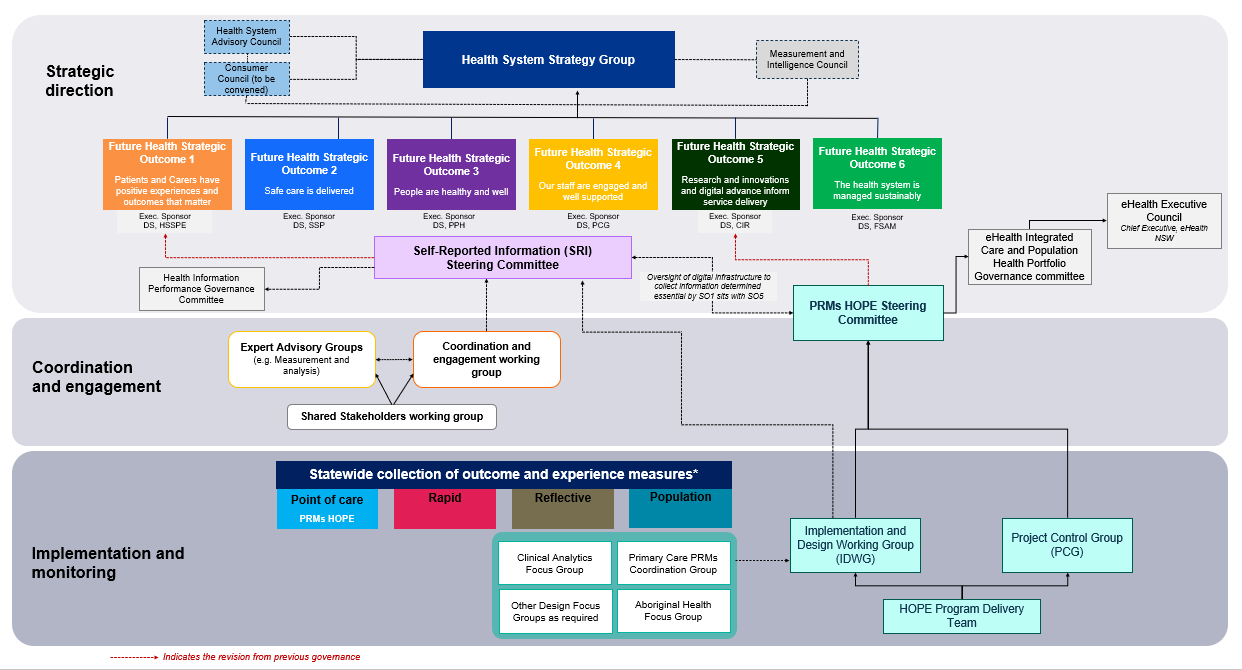
Governance groups are responsible for:
- Endorsing PRMs tools, data elements, definitions, and protocols for statewide use at individual, service, and system levels.
- Ensuring stakeholder input – including priority populations and cultural groups – to shape tool selection and data collection methods.
- Overseeing the HOPE platform’s technical development to meet program needs.
- Guiding the implementation of HOPE across diverse clinical and care settings.
- Advising on education, training, and change management to support HOPE adoption.
- Supporting the effective use of PRMs in clinical practice through training and change strategies.
- Monitoring HOPE development phases, including milestones, risks, budget, benefits realisation and quality assurance.
- Providing strategic advice on statewide PRMs data collection and use, ensuring alignment with the PRMs Framework.
Data governance and management framework
The framework outlines principles for secure, ethical and effective management of PRMs data within the HOPE platform.
Capability framework
The framework defines the skills and knowledge required to collect and use PRMs effectively at the point of care.
Change and adoption strategy
This strategy supports implementation planning and behaviour change to embed PRMs into clinical practice and shared decision-making.
Stakeholder engagement and communications framework
This framework identifies key stakeholders and describes how the PRMs Program team communicates and collaborates across the system.
Accessing PRMs data
If you're a clinician, health service manager or researcher seeking access to PRMs data for analysis or reporting, please refer to the ACI’s data request process.