Spinal Seating Modules
Recognizing key relationships between the client and wheelchair
Four key considerations
1. Excessive time exposure to applied pressure to tissue causes pressure injuries
A pressure injury is a localised degeneration of the skin and underlying tissues, usually over a bony prominence as a result of a sustained mechanical load1, 2. Tissue damage occurs as a direct result of sustained tissue deformation, as a result of extended tissue ischemia, or by a combination of these factors. While different individuals have different tolerance for applied pressure, the higher the applied pressure the sooner tissue damage will occur. If the time exposure to tissue loading is reduced then the risk of pressure injury is also reduced. The figure below shows the risk of cell death (tissue damage) as a function of both time and applied loading.
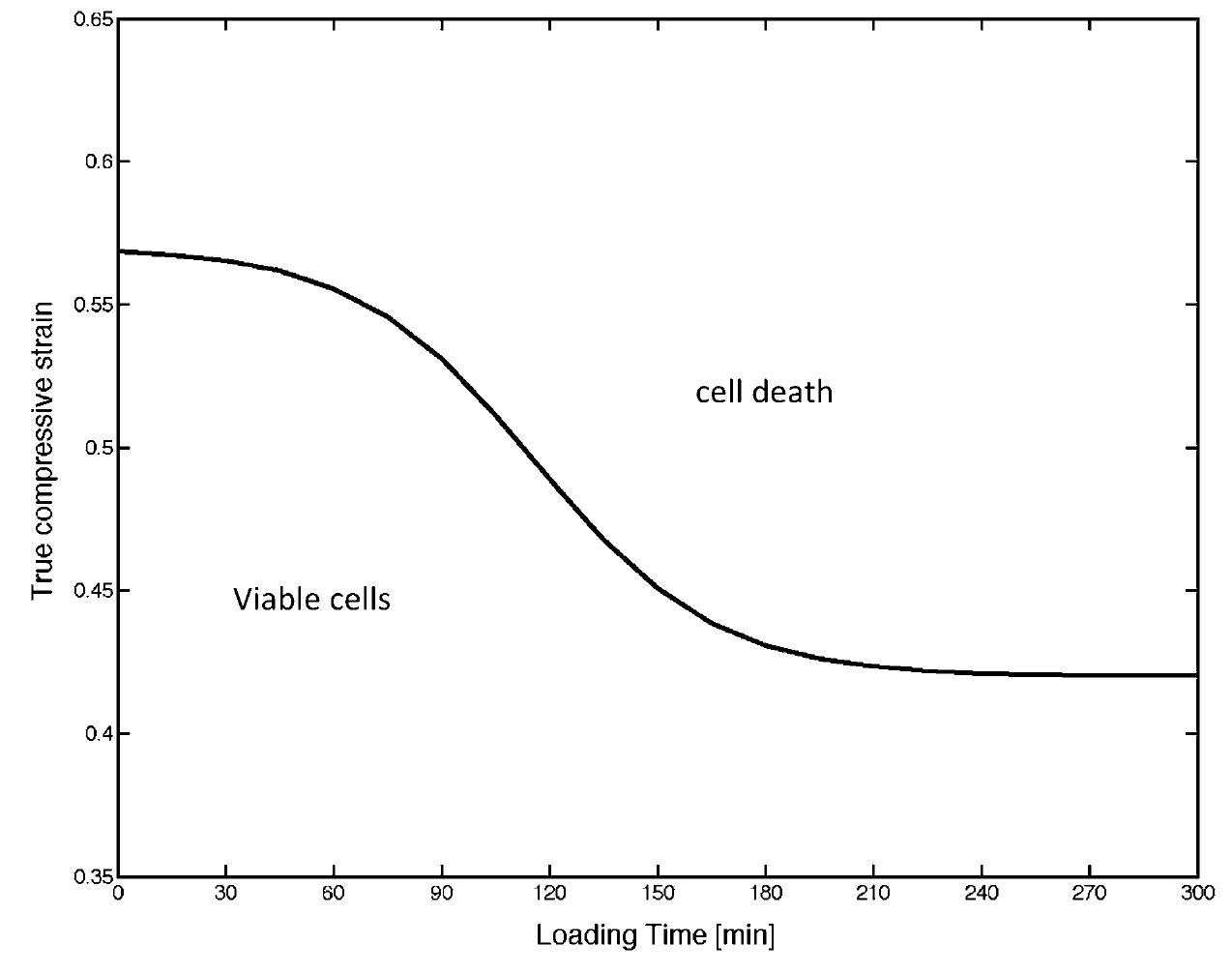
Figure 2: The likelihood of cell death increases when duration/magnitude of tissue loading increases. This figure is a reproduction from Oomens et al. (2014)1, and adapted from Gefen et al. (2008)3.
Lower applied pressures on vulnerable tissue can be achieved by choosing and configuring appropriate equipment but this is often insufficient to fully safeguard tissue and periodic pressure reduction or relief is needed to reduce the time exposure. The term ‘weight-shift’ encompasses various strategies for reducing or fully relieving tissue loading that the client can use to aid in managing their risk of pressure injury. In practice, clients should be able to employ one or more weight-shift strategies independently, from their wheelchair.
2. Pressure management equipment selection needs to be individualised
- Factors contributing to the selection of equipment include:
- Specific individual vulnerability to pressure injury due to variations in skeletal anatomy, history or previous tissue injury, nutritional status, cognitive ability, sensory ability and behaviour,
- Client functional goals
- Comfort requirements and challenges
- Postural challenges for pressure management, and
- Care environment aspects for safe hoisting, transfer, positioning of the client and equipment maintenance.
- Correct selection of support surfaces is critical to a good pressure management outcome, but is not sufficient to ensure a good outcome.
- The relative placement of the body support components determines how they interact with the client’s body, and apparently minor changes in the relative position of parts can have a major effect on the risks of pressure injury. Conversely it may be possible to resolve chronic pressure management problems by modest but significant changes to the configuration of seating and wheelchair components. For example, elevation of foot supports, even by a few centimetres, will raise the knees about cushion support surface, which in turn can increase the pressure on the pelvis and vulnerable bony prominences potentially leading to a pressure injury.
- It takes time to evaluate a proposed combination of support surfaces and system configuration.
- To do this prudently the assessment should start with a short trial, extending the duration in stages, with skin checks at the end of each stage to verify that there is no visible tissue damage.
- The incremental time trial needs to continue until the trial period matches the client’s typical time between occasions of effective weight-shift.
- If skin checks reveal skin marking, the trials should be suspended until the marking resolves. Meanwhile the underlying cause for the marking should be determined and addressed before recommencing trials.
3. Seating configuration is as important as support surface selection for managing pressure injury risk
- Correct selection of support surfaces is critical to a good pressure management outcome, but is not sufficient to ensure a good outcome.
- The relative placement of the body support components determines how they interact with the client’s body, and apparently minor changes in the relative position of parts can have a major effect on the risks of pressure injury. Conversely it may be possible to resolve chronic pressure management problems by modest but significant changes to the configuration of seating and wheelchair components. For example, elevation of foot supports, even by a few centimetres, will raise the knees above cushion support surface, which in turn can increase the pressure on the pelvis and vulnerable bony prominences potentially leading to a pressure injury.
4. Changes in pressure management should be explored conservatively, with incremental time trials of new or changed equipment
- It takes time to evaluate a proposed combination of support surfaces and system configuration.
- To do this prudently the assessment should start with a short trial, extending the duration in stages, with skin checks at the end of each stage to verify that there is no visible tissue damage.
- The incremental time trial needs to continue until the trial period matches the client’s typical time between occasions of effective weight-shift.
- If skin checks reveal skin marking, the trials should be suspended until the marking resolves. Meanwhile the underlying cause for the marking should be determined and addressed before recommencing trials.
Keys to pressure management
The primary aim of pressure management in spinal seating is to provide clients with a stable seating system that provides a distribution of seating pressures that can be sustained without injury for a reasonable period of time. The risk of pressure injury is affected by a range of client specific factors including anatomical variations, lifestyle, environment and circumstances. Determining these factors is covered in Modules 2-5. Therapists can use this information to aid the selection and configuration of appropriate equipment and education of weight-shifting practices to manage seating pressures.
Skeletal anatomy and seating pressure risks
In seating, loading occurs when tissue is compressed between the seating equipment and the skeleton. Clients with SCI typically have significant muscular atrophy below the level of injury, increasing the risk of pressure injury. While the seating equipment can be changed, the client’s skeleton cannot (without surgery). Equipment should therefore be selected to suit the skeletal anatomy of the client.
The ‘size’ and ‘shape’ of the bony features of a client’s skeleton is individual. Tissue around smoother, flatter sections of bone is typically better able to spread loading, while tissue around rougher or pointer sections of bone are more vulnerable to localised high pressures. In seating, this means that tissue around the coccyx and ischial tuberosities is most vulnerable to pressure injury, followed by the less protruding bony prominences such as the greater trochanters and the sacrum. Conversely, tissue around the large, smooth femurs is typically able to sustain greater contact pressures. It is often desirable to configure a seating system to achieve low pressures under vulnerable tissue by increasing loading to areas of tissue that are more resilient.
Variations in postural presentation also affect tissue loading around bony prominences. Pelvic tilt and pelvic obliquity are common postural presentations that have consequences for pressure management. A posterior pelvic tilt may place the coccyx in contact with the seat surface and the ischial tuberosities move forward on the cushion. This must be considered if using a cushion with a defined ischial well. With extreme posterior pelvic tilt the sacrum may also come into contact with the cushion and should be assessed for pressure risk. In the case of anterior pelvic tilt the ischial tuberosities are located more rearward towards the back support. Pelvic obliquities will typically result in asymmetrical pressures, with tissue around the bony prominences on the lower side being more heavily loaded. These postural presentations may require correction or accommodation through cushion design determined through the seating assessment process (see Modules 3-7) and equipment trials.
Pressure management equipment: wheelchair seat cushions
There are many types of wheelchair cushions available, but only a limited range is suitable for clients at high risk of pressure injury.
The seat cushion can assist by redistributing pressure away from the vulnerable bony prominences under the pelvis. There may also be requirements to manage posture, to provide adequate balance and stability, to enhance functional capability and ensure comfort. It is important to consider whether the cushion will be able to survive the rigours of daily use and suits the client’s ability to adjust and maintain the cushion.
Cushion design strategies to limit peak pressures generally include the concepts of immersion (allowing the body to sink into the cushion), envelopment (conforms to the shape of the body), and cushion pre-contouring.
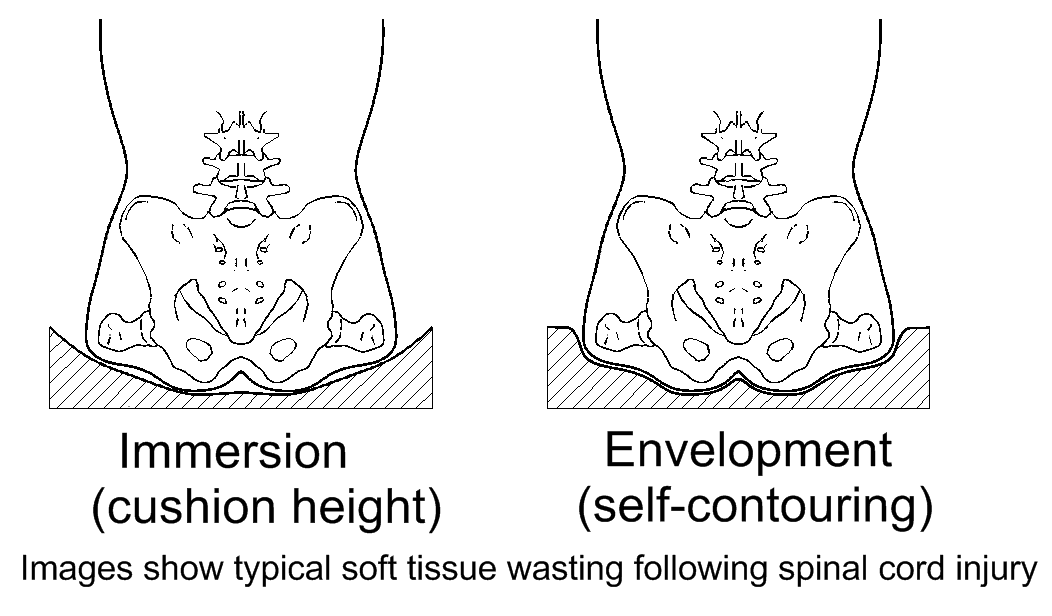
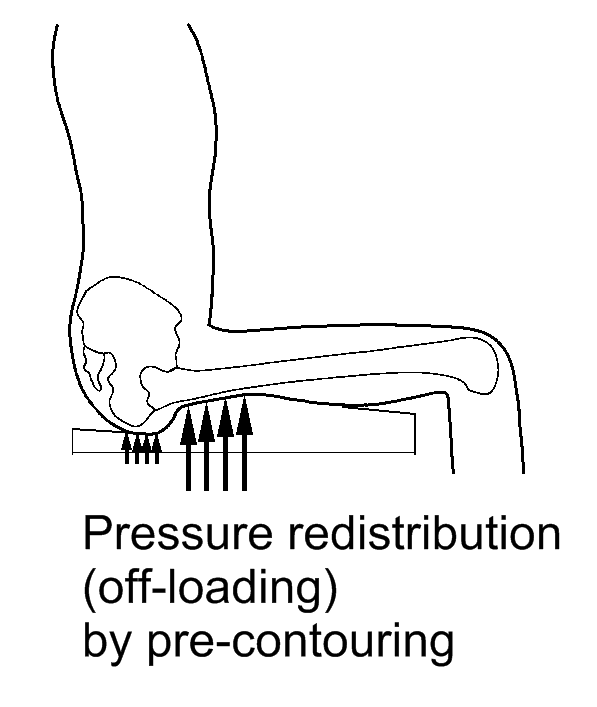
Pressure management strategies used in cushion design.
| Definition | Benefit |
|---|---|---|
Immersion | The degree to which a support surface allows a body to ‘sink’ into it. | Sinking into the support surface increases the area of contact between the body and the support. This reduces the average contact pressure; local pressures should still be check (especially around vulnerable sites). |
Envelopment | The degree to which a support surface locally conforms to the contour of the body. | Allowing the support surface to conform around bony prominences reduces localised pressure. |
Redistribution | Use of material properties and contouring on a support surface to transfer pressure from one region of tissue (usually a high risk site such as tissue over a bony prominence) to another (typically a low risk site) | Allows targeted pressure reduction around high risk tissue. Can be used very effectively but often requires greater accuracy in seating position to ensure contouring/materials are in the intended position relative to the body. |
While these concepts help us understand cushions properties for pressure management, cushion evaluation should be individualised to encompass all of the client’s seating goals where possible.
Cushions providing immersion for good pressure management need to be thick enough to prevent the ‘bottoming out’ of the bony structures on the base of the cushion with high pressure contact. For cushions available in various thicknesses, it is generally the case that thicker options have more potential for good pressure management.
Cushion manufacturers rate their products for pressure management performance. These ratings are not comparable between manufacturers, but do give some guidance as to the relative performance of cushions within the manufacturer’s range.
Some types of cushions that are successfully used for pressure management of clients with SCI are:
- Fluid gel sacs with a contoured foam base.
- Air cell cushions, with or without a contoured foam base
- Flexible foam, often contoured, and
- Other cushion types suitable for individual clients.
Fluid gel with contoured base (e.g. Jay fluid, etc.)
These come in a variety of thicknesses and styles. The hard foam base is contoured to offload the most vulnerable bony prominences, and add load to the structures best able to take pressure. The contouring creates a well under the pelvis, and the well is fitted with fluid gel sacs which are self-contouring to follow the body shape. The fluid gel sacs are confined to the pelvic well, and other parts of the upper surface, including the greater trochanter and thigh areas, are padded with flexible foam.
This construction offers good postural support and stability, but there are limits on postural variations and asymmetries that can be accommodated. For example, users with a forward placement of the pelvis on the cushion can experience pressure problems if the tuberosities contact the front of the pelvic well.
For users of manual wheelchairs who need to lift the cushion from the chair, fluid gel cushions have the disadvantage of being comparatively heavy.
The fluid gel needs little maintenance apart from regular kneading and smoothing to eliminate any deep hollows before transferring the user on to the cushion. When in use the fluid gel is reasonably protected from environmental hazards.
Over time the fluid gel changes its viscosity and loses volume. This can ultimately results in the user bottoming out on the cushion base with consequent pressure marks and possible pressure injuries. The manufacturer of Jay cushions recommends replacement of cushions every three years. It is possible for the fluid gel sac to leak, but this is unusual.
Air cell cushions (e.g. Roho, Star, etc.)
These have the whole sitting surface made with interconnected air cells so that the whole cushion is self-contouring to the shape of the user. The basic cushion (with all cells interconnected) allows the user some variation in placement on the cushion and in pelvic posture while maintaining good pressure management. If the user leans to one side the air can move to the other side of the cushion and this can unbalance some users, so alternative versions of this cushion type have the air cells grouped in separate zones to improve the stability and balance of the user.
The self-contouring design and soft surface creates a high level of comfort that best suits some users.
Air cell cushions need correct inflation to be effective and safe. Clients (or their carers) must be vigilant in checking cushion inflation and proficient in adjusting the cushion inflation when required. Some air cell cushions have additional components that can assist users to monitor the inflation of their cushion. Assessing the capability of the client and carers to manage the cushion long term is a necessary consideration when prescribing an air cell cushion.
Some users find air cell cushions difficult for self-transfer, because unlike a firm cushion, the user’s hands sink to the level of the cushion base during transfer.
A significant consideration for air cell cushions is their potential for puncture, leading to a complete loss of the cushion’s pressure management capability. The environment of use may be a concern if there is a high risk of puncture. Industrial situations with sharp objects or fragments, pets prone to clawing or biting the cushion and cigarette burns are known risky situations.
Air cell sections with foam base(e.g. Roho Hybrid, Jay Fusion (Air)) are a variant of air cell cushions. These cushions are similar in concept to fluid gel with foam base, but use air cells instead of fluid gel sacs.
Compared with an air cell cushion without a contoured base, this system:
- Gives more stability and more specific postural support to the body
- Is less forgiving of postural and positioning variations, and
- Is easier for self-transfer because the front part (where hands are often placed for support) has a firm surface.
Flexible foam (e.g. contoured foam cushion)
Cushions made using flexible foam (and similar flexible materials) are generally contoured to achieve pressure management by offloading vulnerable structures. Flat (uncontoured) foam cushions have limited capacity for pressure management.
Foam is light and reasonably durable. While there is no risk of immediate catastrophic failure (such as a puncture), flexible foams slowly become softer with continued use and eventually become ineffective for purpose. Typically the life of a foam cushion is one to two years. Few commercial foam cushions claim to offer high level pressure management but it is possible, usually by custom making to client needs, and cushions of this type are available from NSW Spinal Seating Services. A high level of clinical skill is necessary for successful assessment and prescription of contoured foam cushions (either commercial or custom made).
Other cushion types
There is a broad range of cushions, many of which claim to be suitable for clients at a high risk of pressure injury. Regardless of the manufacturers claims any equipment that is proposed for a client should be trialled in a careful, conservative, incremental manner, to verify appropriateness for the intended client. Many high care cushions have some contouring or variation of material under the bony prominences, when prescribing a cushion ensure that, as far as possible, the item being prescribed has been trialled (same model, size, features and cover type).
Cushion covers
The cushion cover is an important part of the cushion. The cover needs a soft, stretchy material on the sitting surface to allow the user to sink into the cushion, and to avoid excessive tension in a stretched cover, which increases pressure under bony prominences. A cover which is stiff or inflexible does not allow for envelopment (local pressure relief).
In the case of some cushions, a portion of the pressure management material is integrated into the cushion cover. A pressure management cushion should therefore always be fitted with the manufacturer’s cover to ensure the full benefit of the designed pressure management.
Cushion manufacturers offer special covers to address specific issues including incontinence, excessive heat and sweating. These special covers have varied properties which may reduce the pressure relieving capacity of the cushion as a whole. Cover properties also influence the microclimate for skin in contact with the cover, the amount of shear that develops when the user attempts to slide on the cushion.
Material placed between the client and the cushion may reduce the effectiveness of a pressure care cushion. This includes non-stretchy clothing, cushion overlays, sheep skins, hoist slings and incontinence pads.
Pressure management equipment: configuration of seating and wheelchair
To achieve good pressure management a wheelchair and seating system should always be ‘configured’ to suit the individual client. Configuration refers to the relative positioning of all parts of the wheelchair and seating system that support the body.
Refer to the body measurement (Module 4) to determine the appropriate size of the support surface such as cushion, backrest and arm supports, to maximise contact surface for weight distribution. Wheelchair frame size, arm supports and foot supports dimension and configuration are critical in supporting postural alignment and stability (refer to Module 5 and Module 7).
Cushions and backrests are customised to an appropriate shape for the client according to the findings of postural assessment (Module 3) and postural interventions (Module 7).
Postural intervention aims to:
- Achieve a symmetrical posture, where possible, which can also have benefits for pressure management, and
- Provide a stable posture and reduce undesired movement of the bony prominences on the support surfaces.
Seat Depth
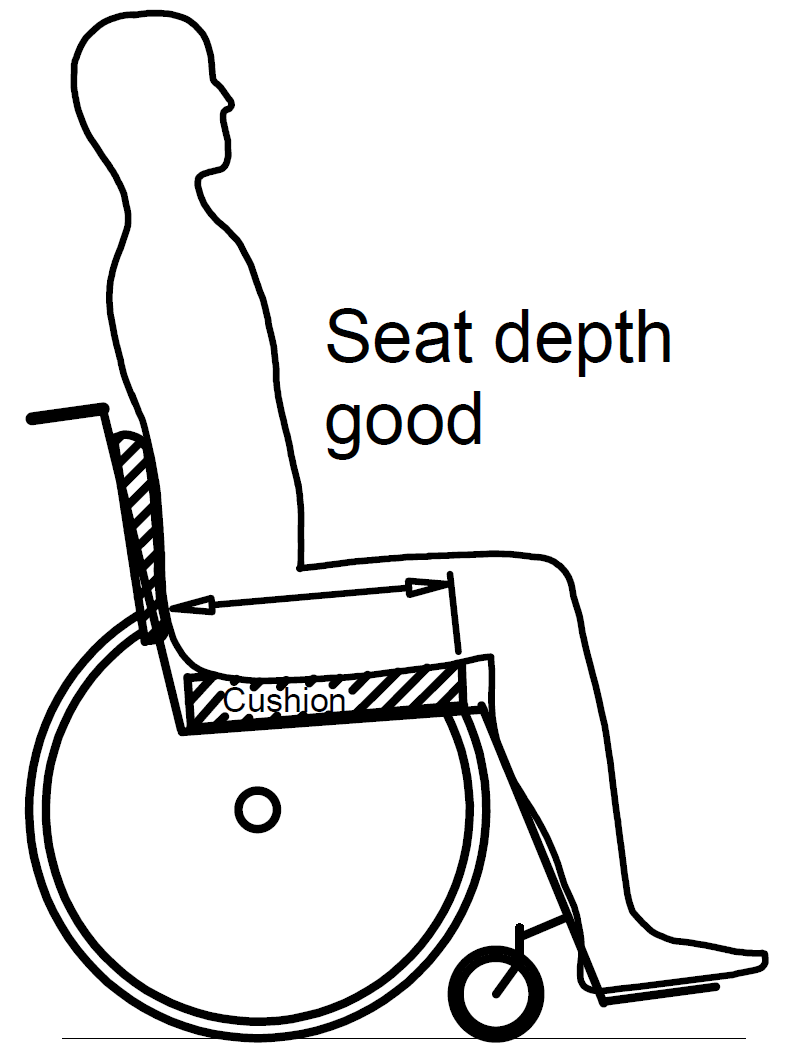
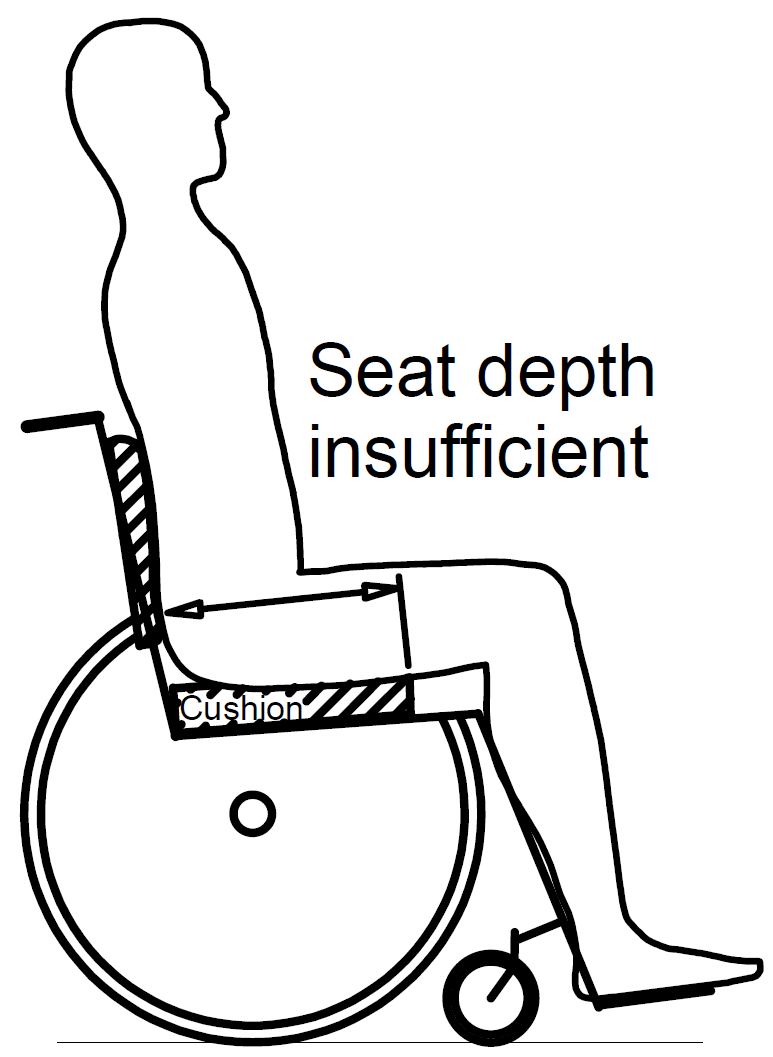
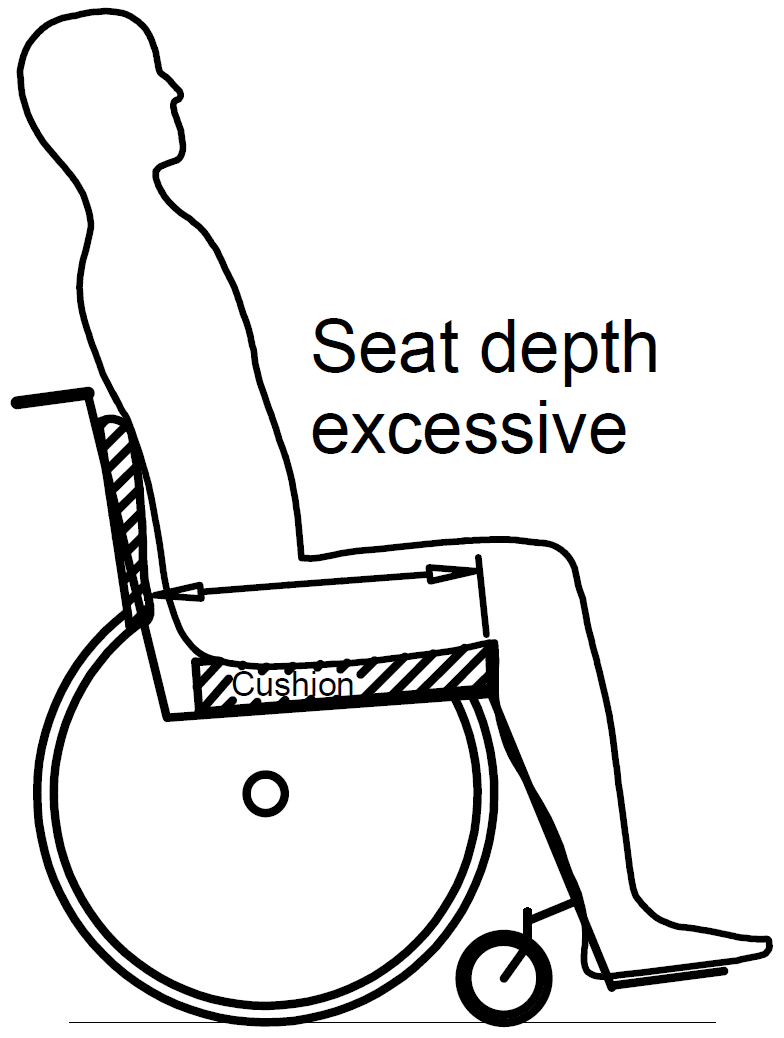
It is recommended that a clearance of greater than 0.5 inch /14mm exists between the front edge of the cushion and the popliteal fossa, with a clearance of 5cm being typical. Client’s whose seating results in a thigh-to-lower knee angle of less than 90 degrees, or who need to hook their arm under their thigh from the front for transfer may require greater clearance to meet these needs.
If the seat depth is longer than the buttock-to-thigh measurement (sacrum to popliteal fossa), there will be contact with the back of the calf which may result in the pelvis being pulled into posterior tilt.
Seat depth affects the available area of contact between the client and the seat. Increasing this available area will reduce the average seating pressure across the seating tissue but may not improve pressure management at the critical bony prominences. As with any change in seating configuration or equipment, clinicians should evaluate the effect of changing seat depth with conservative, incremental time trials.
It is important to check that the body does not overhang the rear of the cushion and thereby remove an important area of support. This problem may be difficult to see when the client is seated. In some cases the lateral wings of a deeply contoured backrest may interfere with the cushion and prevent it from being moved back to the correct position.
A similar lack of support can occur if the cushion overhangs the rear of the seat board (or seat sling in the case of a manual chair).
Seat width
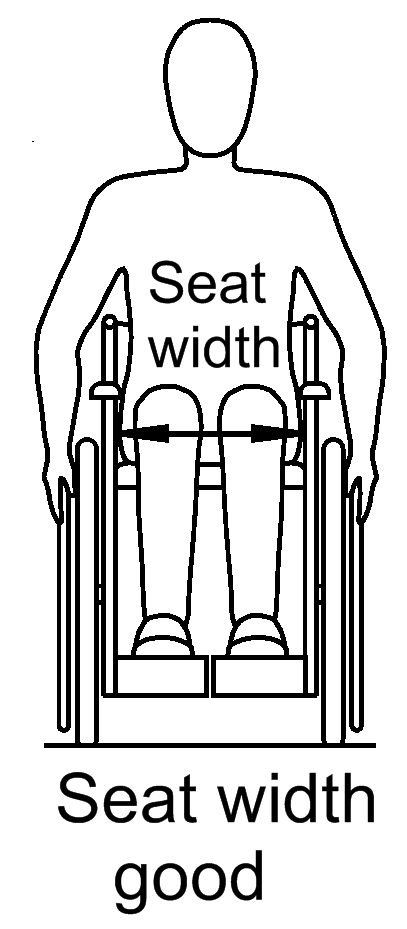
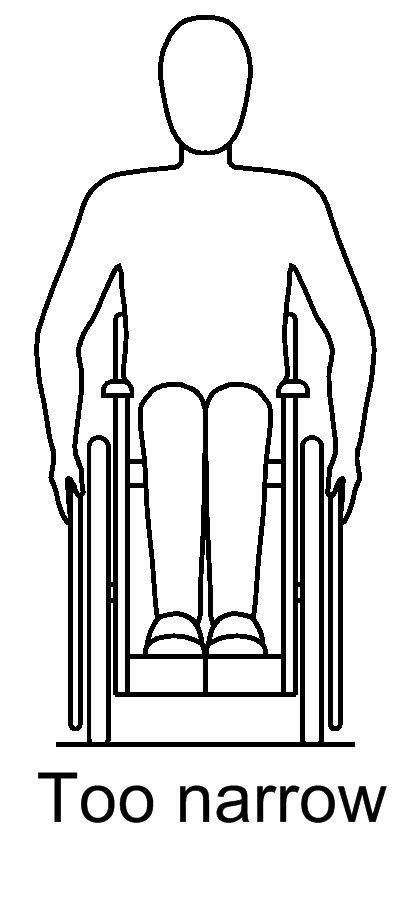
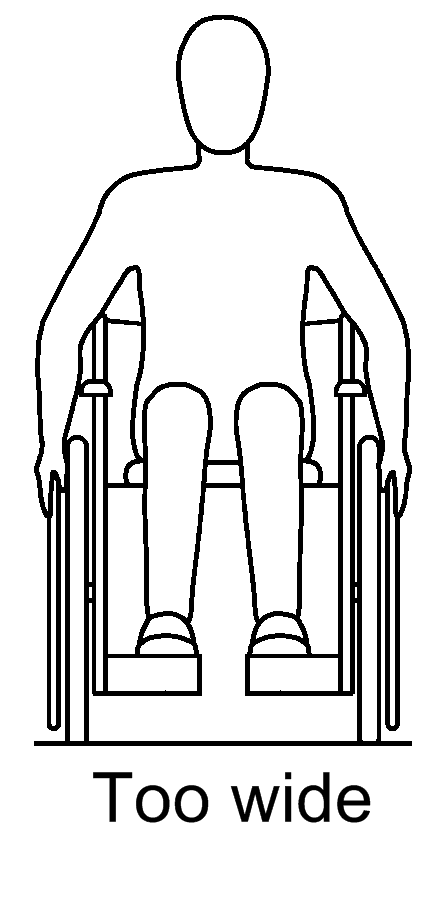
A chair with the correct seat width can help to maintain postural stability and constrain some asymmetrical presentations such as pelvic rotation and obliquity. Excessive seat width may result in the client leaning toward the joystick to operate the power wheelchair, creating a poor postural pattern.
If the seat is too narrow, there may be localised pressure against the greater trochanters or grazing of the skin or clothing by the push wheel.
The width of the cushion needs to be assessed with respect to the client, and not just the width of the chair. Refer to the information provided by cushion manufacturers to size the width of the cushion correctly. E.g. some cushions with a pelvic well require specific skeletal measurements to ensure sizing of the cushion for optimal pressure management.
Seat to foot rest distance (footplate height)
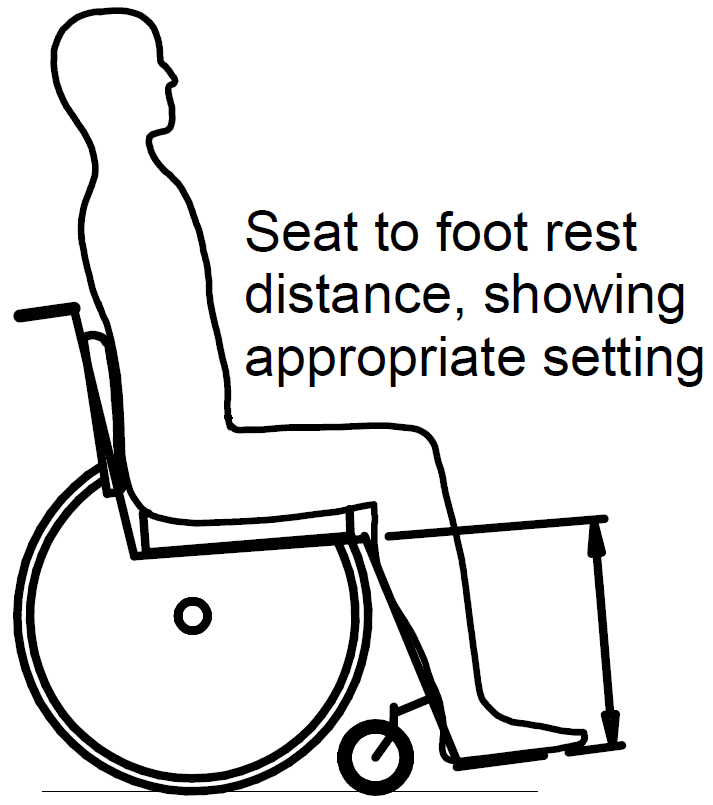
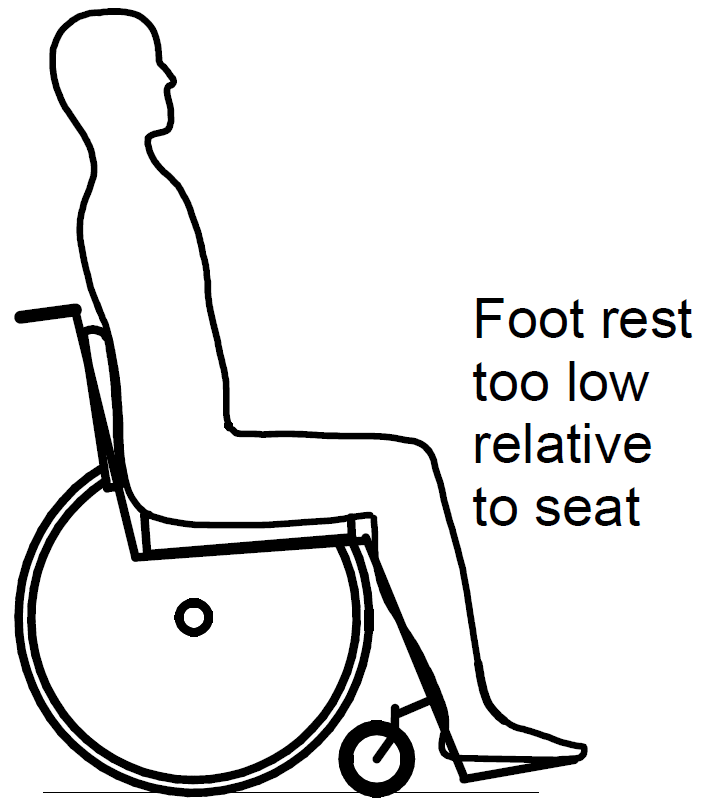
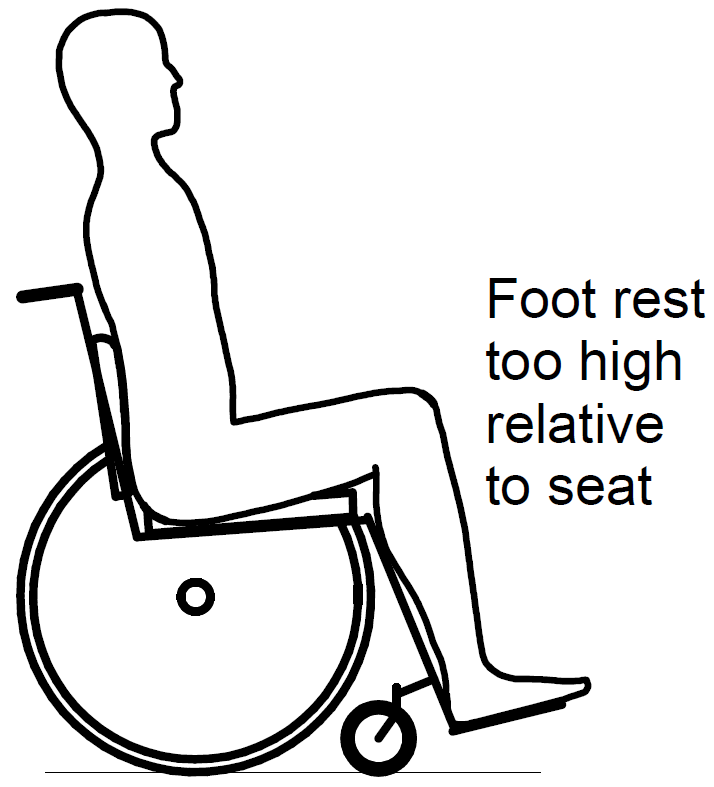
Wheelchair foot supports are intended to support the feet to prevent the development of fixed deformities. Optimal foot support height also relates to pressure management.
Raising the foot supports above the optimal position will elevate the thighs and can raise pressure under the feet as well as under the pelvis, typically on bony prominences such as the ischial tuberosities or coccyx.
Lowering the foot supports below the optimal height may encourage the pelvis to move forwards. Excess pelvic posterior tilt can result in an increase in tissue loading on the coccyx and sacral areas. A forward movement of the pelvis may place the Ischial tuberosities against the firm front slope of the pelvic well of some cushions and increase pressure risk.
Backrest/back support:
For chairs with seat tilt or backrest recline capacity, the body weight is transferred onto the backrest in the tilted or reclined position, so the backrest support should be contoured to the shape of the client to maximise the support area. It should be chosen to achieve the preferred posture and balance determined in the MAT evaluation.
Extra padding or local depressions may be needed for pressure management of vulnerable bony prominences on the back, such as spinous processes, scapulae, or posterior superior iliac spine (PSIS).
Arm support /armrest height:
In a typical neutral sitting posture the armrests generally support 5- 9% of body weight5.
Armrests play an important part in postural alignment and assist with body weight distribution. The height of the armrests should be adjusted to support the elbows without elevating the shoulders. Having the armrests too low can result in subluxation of the shoulders if the client cannot support the weight of their arms. Armrests which are set too high will lead to increased muscle strain in the shoulders resulting in pain and reduced mobility of the shoulder joint.
Armrests may require special padding or relief at the elbow to manage pressure vulnerabilities.
Head support / headrest:
A head support is particularly important when the wheelchair is in the tilt or recline position. Headrests are recommended for all wheelchair users travelling in motor vehicles. A headrest provides support to the head and neck throughout transport and may reduce the severity of injuries in the event of an accident.
Weight-shifting strategies
Pressure relief of adequate duration allows blood flow and tissue perfusion to be re-established. Weight-shifting is local pressure relief achieved via postural change or mechanical repositioning of the seating system.
The duration for weight-shift posture should be at least 1 to 2 minutes every 30 minutes1.
There are two types of weight-shifting: independent weight-shifting (where the client physically moves themselves to relieve pressure from vulnerable tissue), and assisted weight-shifting using the functions of the wheelchair.
Independent weight-shifting
This is intentional movement by the client to alter posture so sitting pressure on vulnerable tissues is temporarily reduces or relieved. Common weight-shift manoeuvres include forward lean, side lean, or pushing up with the arms. Clients should be informed of potential problems with safety, respiratory, bladder compression and autonomic dysreflexia as a result of active weight-shift activity. Some clients may choose to be assisted by a carer in using these techniques.
Consider the following points when choosing an active weight-shift strategy:
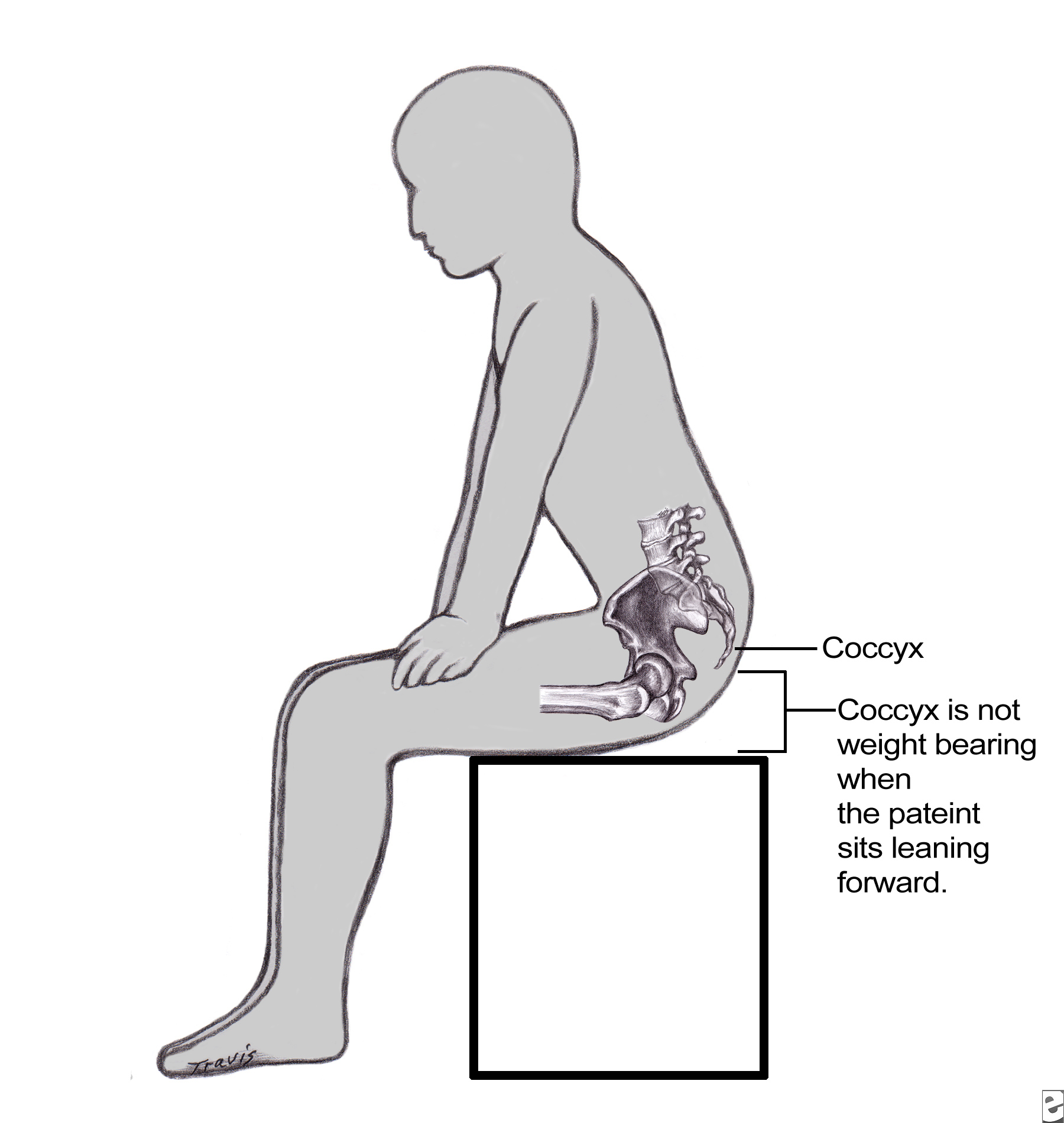
Forward lean

Original line drawings used with permission from Sprigle, S.11
A forward lean (e.g. resting elbows on knees / table in front) can effectively relieve pressure on the ischial tuberosities, coccyx and sacrum.
- Assess the client’s ability to perform weight-shift and to regain sitting position. It is not suitable for clients who are dependent sitters or have limited hip flexion range of motion.
- Consider options such as leaning forward to prop elbows on the knees, or rest on a table to minimize the effort required to maintain the position.
- Discuss strategies for adopting this posture regularly, e.g., during commercial break while watching TV, doing computer work at a work station.
- For safety, apply the wheel locks in a manual wheelchair, or turn power off in power wheelchair before attempting a forward lean.
- With a manual wheelchair, trial forward lean safety with an assistant holding the push handles to prevent forward tipping of the chair (especially with a compact fixed frame manual wheelchair).
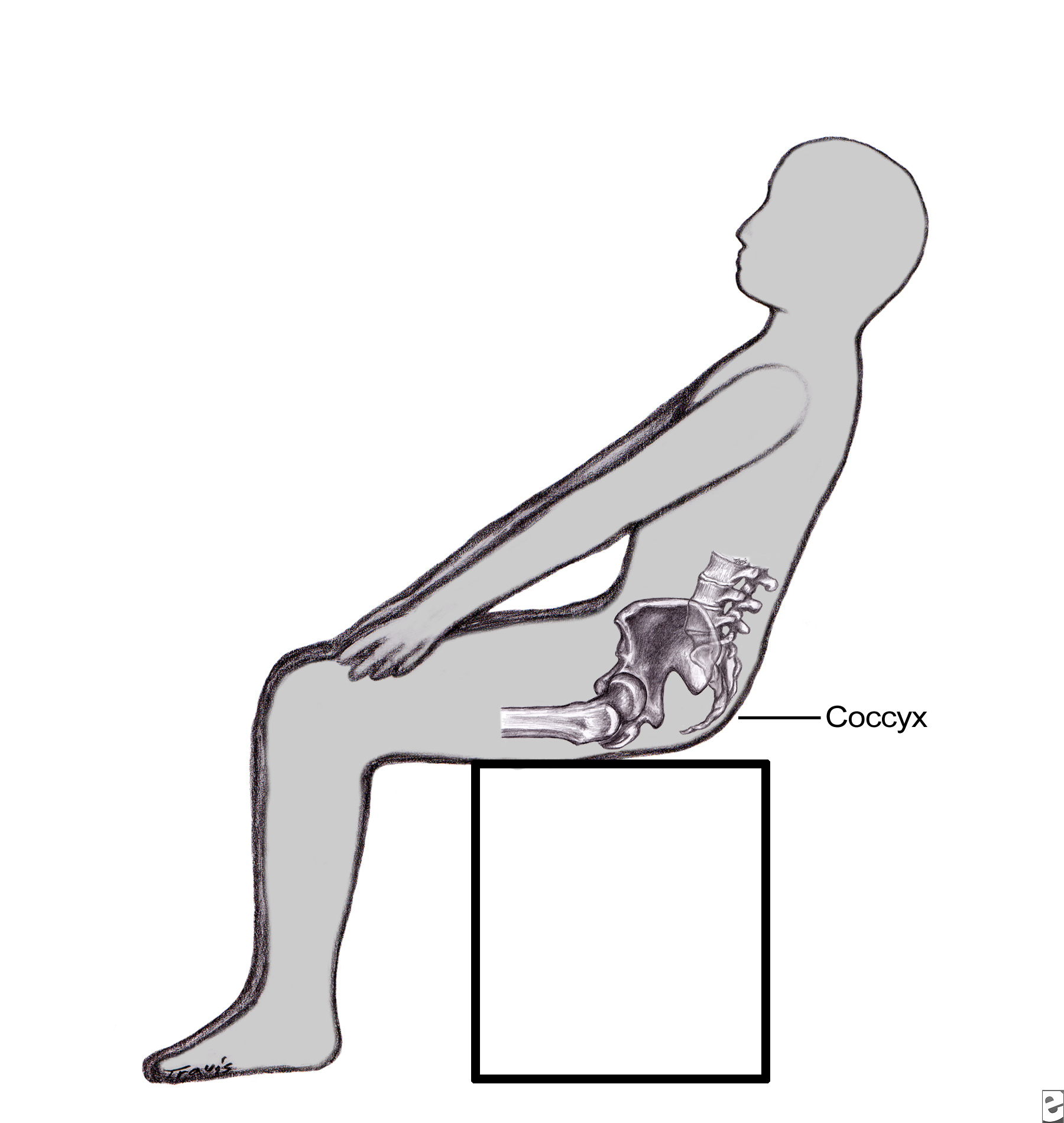
Side lean

Original line drawings used with permission from Sprigle, S.11
- Assess the client’s ability to perform weight-shift and to regain sitting position.
- For safety, apply wheel lock in manual wheelchair or turn power off in power wheelchair.
- Assess seating and wheelchair components for weight-shift:
- Suitable height of the back post (back canes) for hooking an elbow around the push handle.
- Stability of the wheelchair and components when clients hold onto one wheel rim or arm support, then lean to the other side.
Push up on armrest or rear wheels
- Note: the ‘push up’ technique is the least preferred independent weight-shifting techniques as it may contribute to shoulder and wrist pain and injury. It loads the joints in the upper extremity with the upper body weight and many clients find it difficult to sustain the recommended duration of weight-shift (1 to 2 minutes).
- Clients with cardiac conditions should seek medical advice before using this technique.
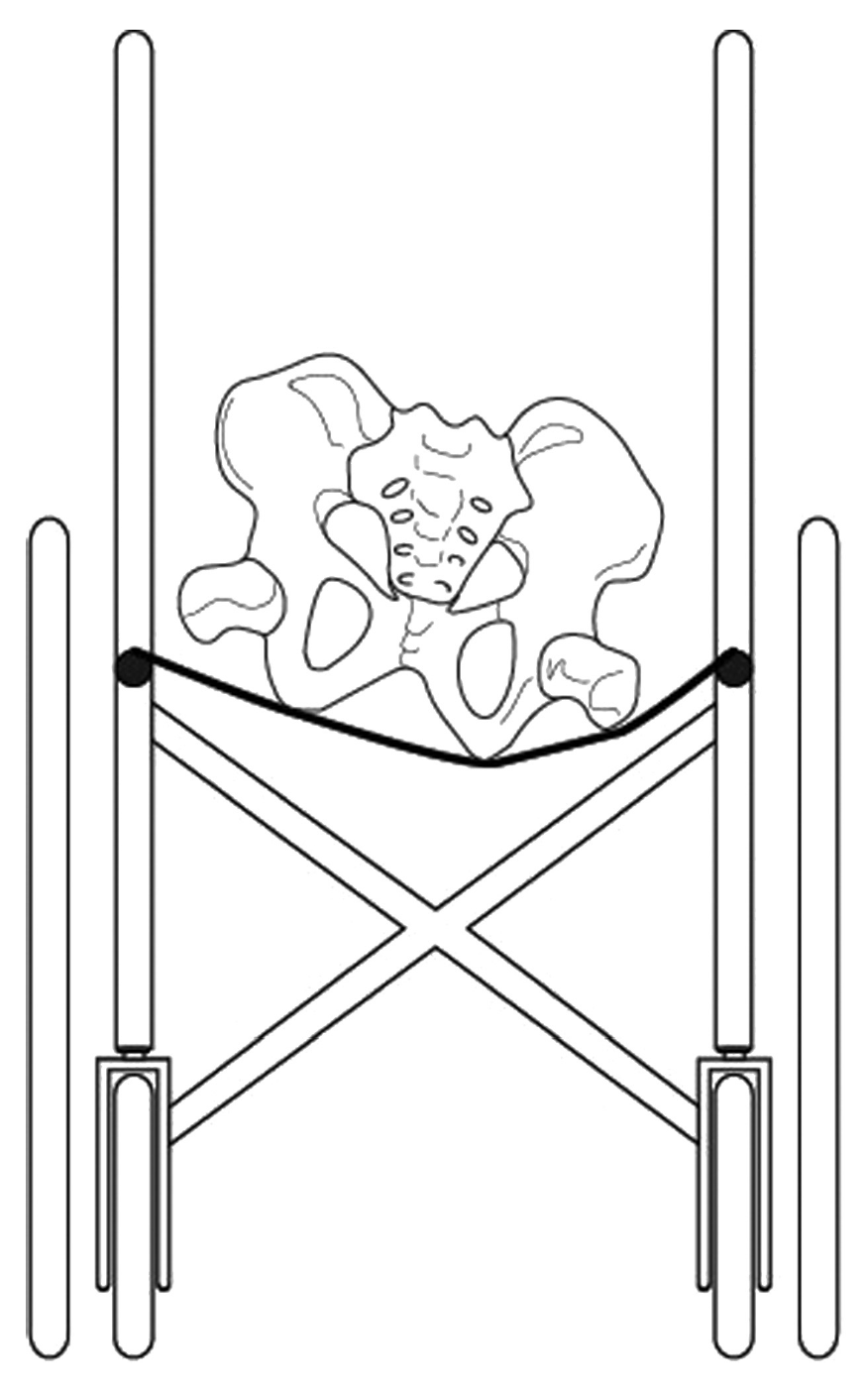
Assisted weight-shifting

Optional features on power wheelchairs assist the client to alter the seating position to reduce sitting pressures by redistributing pressure to other support surfaces. The client can independently operate seat tilt, backrest recline, leg elevation or standing function; depending on the options fitted to the chair.
- During ‘tilt-in-space’ (the whole seating system tilts rearwards), a portion of the body weight is redistributed from the seat onto the backrest and other support surfaces
- In general, at least 30 degrees of tilt is required in order to gain benefits of pressure redistribution. As the tilt angle increases, pressure under the pelvis decreases and with most clients excellent pressure reduction can be achieved with angles of tilt over 45 degrees. Note that this is not effective for all clients.
- Assess all seating support surfaces in the tilted and/or reclined position. Pay attention to back support, head rest, arm support, lower leg support and heel loop.
- Ensure the client has sufficient upper limb control against gravity to operate the tilt control in all positions of tilt. If required, provide upper limb positioning or additional switches to operate tilt, or adaptation to the controller system to operate tilt. For example, a joystick can be configured to use a pull action instead of push to return from a tilted position for those with limited elbow extension.
- With some clients, seat tilt with backrest recline is more effective pressure management than tilt alone. When using a combination of seat tilt and backrest recline for pressure management it is important for the client to correctly sequence these operations to avoid being pushed forward on the seat, as follows:
- To assume weight-shift posture: tilt first, then recline backrest.
- To regain upright position: backrest up and then un-tilt.
- If legrest elevation is considered for prescription with seat tilt and backrest recline, therapists should first assess the client’s range of motion at hips and knees. In this case the sequencing for power functions is as follows:
- To assume weight-shift posture: tilt first, then recline backrest, then elevate legs.
- To regain upright position: legrests down, backrest up, and then un-tilt.
- Education should be given to use power seating functions frequently to their full potential for pressure management. Practice tips include – setting a reminder with a timer at the phone or computer, and weight-shift during television commercials. Some power wheelchair controllers have a timed reminder function.
- With manual wheelchairs, useful weight-shift can be performed manually by an assistant, for example by tilting the seat or reclining the backrest. For manual wheelchair with tilt-in-space and/ or backrest recline mechanisms, clear labelling or safe operating instructions for carer is vital.

References
- Oomens C.W.J., Bader, D.L., Loerakker, S., and Baaijens, F. (2014) Pressure induced deep tissue injury explained. Annals of Biomed. Eng., Feb 2015, Vol. 43, Iss. 2, pp 297-305.
- National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: clinical practice guideline. Washington DC: National Pressure Ulcer Advisroy Panel, 2009.
- Gefen, A., B. V. Nierop, D. L. Bader, and C. W. J. Oomens. Strain-time cell-death threshold for skeletal muscle in a tissue-engineered model system for deep tissue injury. J. Biomech. 41:2003–2012, 2008.
- Wheelchair positioning ( page 58- 62), Pressure Injury Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Professionals, 2ND edition, Consortium for Spinal Cord Medicine, 2014 http://www.pva.org/atf/cf/%7BCA2A0FFB-6859-4BC1-BC96-6B57F57F0391%7D/CPG_Pressure%20Ulcer.pdf#page=74
- Wheelchair support surface page 62 – 65, Pressure Injury Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Professionals, 2ND edition, Consortium for Spinal Cord Medicine, 2014 http://www.pva.org/atf/cf/%7BCA2A0FFB-6859-4BC1-BC96-6B57F57F0391%7D/CPG_Pressure%20Ulcer.pdf#page=78
- Gilsdorf P, Patterson R, Fisher S. Thirty-minute continuous sitting force measurements with different support surface in the spinal cord injured and able-bodied. J Rehabil Res Dev [Internet]. Fall 1991 [cited October 2015];28:33-8 . Available from: http://www.ncbi.nlm.nih.gov/pubmed/1941647
- Measure It: Proper Wheelchair Fit Is Key to Ensuring Function While Protecting Skin Integrity” Stephen Sprigle PhD, PT
- Seating system for people with spinal cord injury: assessment, prescription and other considerations – information resource for service providers “Queensland Spinal Outreach Team, 2013 https://www.health.qld.gov.au/qscis/documents/seating.pdf
- Translating evaluation measurement to wheelchair dimensions”, Invacare http://cdn2.hubspot.net/hub/287403/file-663602043-pdf/Get_Back_In_Game/13-488_WC_Measurement_Guide.pdf?t=1402685575651
- Page 60, Pressure Injury Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Professionals, 2ND edition, Consortium for Spinal Cord Medicine, 2014 https://www.mascip.co.uk/wp-content/uploads/2015/05/CPG_Pressure-Ulcer.pdf)
- Sprigle S, Sonenblum S. Assessing evidence supporting redistribution of pressure for pressure ulcer prevention: A review. J Rehabil Res Dev. 2011; 48(3):203-14. DOI:10.1682/JRRD.2010.05.0102
- Position Changes for Managing Sitting Pressure/Postural Issues, Fatigue and Discomfort” - The Spinal Cord Injury Research Evidence (SCIRE) Project https://scireproject.com/evidence/rehabilitation-evidence/wheeled-mobility-and-seating-equipment/pressure-mapp