Spinal Seating Modules
The mechanical assessment tool (MAT)
The MAT is commonly used by seating clinicians as part of the seating assessment process. It may also be referred to as a biomechanical assessment and physical evaluation.
The MAT is a musculoskeletal examination of the client's:
- Range of motion
- Joint flexibility
- Muscle length, and
- Skeletal alignment.
It usually involves postural assessment of the person in their existing seating system, in supine, and sitting on a firm surface. Neurological issues such as tone and spasm pattern should be noted as they affect posture and muscle length.
Limited muscle length or joint flexibility can restrict the client’s seated posture. Functional capacities such as arm reach to the controls, or propulsion of a manual wheelchair may also be affected.
Tone and spasm may become evident whilst conducting the MAT. An assessment task may be halted during an intense spasm and can be resumed when it subsides. Spasm can be triggered by internal stimuli such as urinary tract infection or blocked catheter, or external stimuli such as rough terrain or a change in backrest angle. Unsupported posture during spasm may place the client at risk of falls or lead to the development of postural deformities.
The MAT process facilitates the selection of a seating system with appropriate ‘size’ and ‘shape’ for the client. This is done with respect to the client's requirement for functional capacity, posture and pressure management.
Clinical knowledge required to conduct a MAT
In order to conduct a MAT a therapist will need to be able to:
- Locate bony landmarks of the pelvis
- Understand the structure of the client’s skeleton and the influence of the various muscle groups on the articulation of the joints.
- Understand body planes and ranges of movement to identify fixed vs. flexible deformities.
Bony landmarks of the pelvis
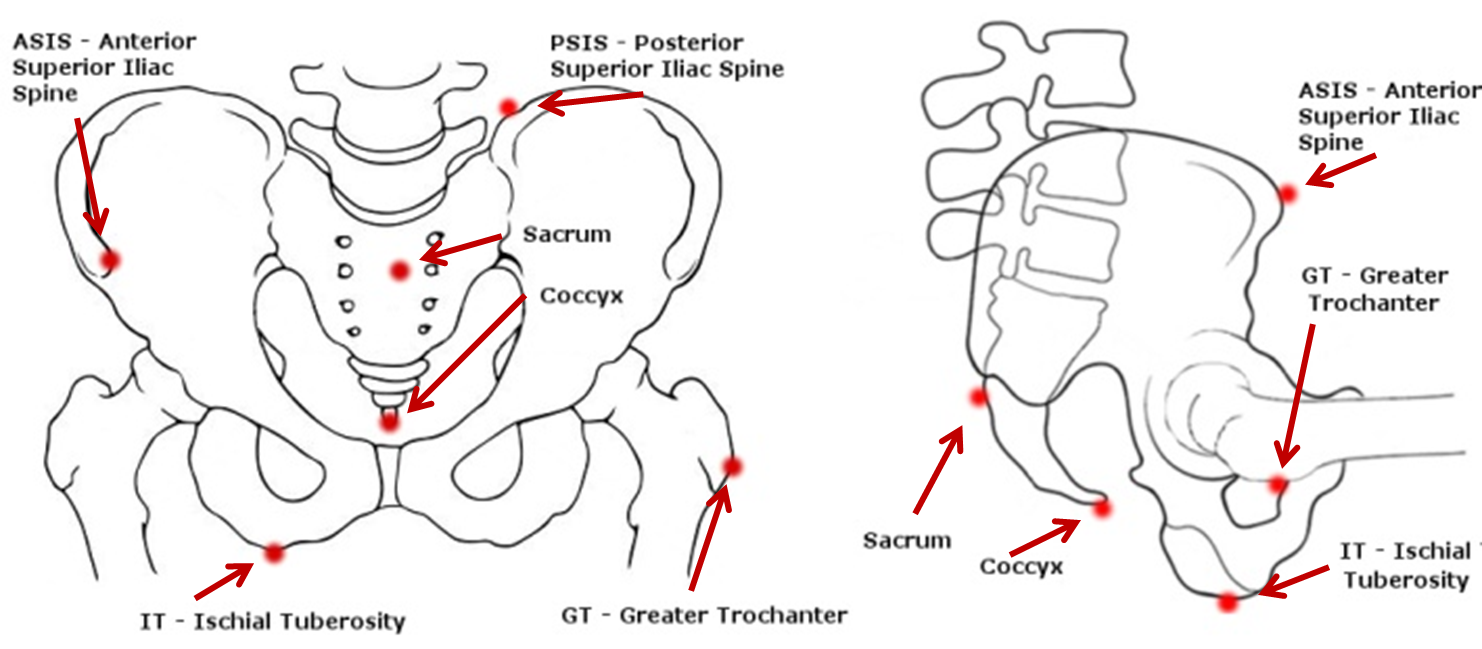
Figure 1: Bony landmarks of the pelvis.
Level of injury, sitting balance and seating
Clients with a spinal cord injury may require seating support due to reduced or absent nerve innervation to the abdominal-thoracic muscles that provide intrinsic postural support for independent sitting. Other factors, such as "completeness/ incompleteness" of the SCI, upper extremity injury, co-morbidities and orthopaedic complications can also influence balancing tasks.
A general guide to seating balance for clients with a complete spinal cord injury
Low thoracic-level T9-T12 and lumbar/sacral-level injuries
Hands-free sitters can sit without using their hands for support and can change their sitting posture.
- The seating system may include a low backrest/posterior support, contoured cushion, customised backrest and seat angles of the manual wheelchair optimised for pelvic stability and skeletal alignment, and for efficient and comfortable propulsion
- Assessment of sitting balance skills should also cover the use of manual wheelchairs in propulsion and in reaching tasks.
High thoracic-level T1-T8 injuries and lower cervical-level C5-C8
Hands-dependentsitters need at least one upper extremity for support or otherwise adopt a ‘C-sitting’ posture to compensate for balance when both arms are lifted simultaneously.
- The seating system may include posterior and lateral postural support while maintaining neutral lordosis and kyphosis position
- The assessment of static posture and dynamic balance varies greatly with the level of spinal cord injury. Consider physiotherapist assessment/reports, activity level, time since injury and appropriate functional task such as feeding (hand to mouth movement), emptying catheters, reaching task, transfer and wheeled propulsion (refer to the initial interview form, see Module 2). This approach will contribute to determining whether the seating system can be configured to improve sitting balance, freeing the upper limbs for functional tasks.
High cervical-level C1-C4 injuries
Dependent sitters (also referred to as propped sitters) are unable to support themselves in sitting using the trunk muscles and upper extremities.
- External supports are required for total body support including upper thoracic, armrests (and possibly headrests) to maintain an upright sitting posture
- Most propped sitters use power seating and wheeled mobility systems for independent mobility, postural and pressure care management.