Spinal Seating Modules

Spinal seating: Overview
While all spinal cord injuries (SCI) involve some degree of damage to the nerves within the spinal cord, the severity, level and resulting loss of function varies greatly. This variation can make spinal seating a complex problem solving exercise, especially when determining the specifics of a client’s situation and finding a solution that best meets their individual needs. Generally all people with SCI have some degree of motor or sensory loss and a disrupted autonomic nervous system. This has a profound effect on a person's health, function and physiology.
The global incidence rate of SCI is estimated to be 40-80 cases per million people.1
More than 80% of individuals with SCI will be affected by pressure injuries.2
20-30% of people with SCI will also struggle with clinical depression.1
Clients with SCI are 2 to 5 times more likely to die prematurely than the average.1
The most important factors predicting functional outcome are the neurological level and degree of completeness of spinal cord lesion. As the neurological level becomes lower, functional independence should increase.
A range of other medical and non-medical factors can influence outcome, including:
- Age
- Body shape and weight
- Associated injuries
- Pre-existing disease
- Spasticity and contractures
- Living arrangements and family support
- Level of education and
- Financial resources.
These factors can all determine which seating intervention approaches can be pursued and which are inappropriate. Each client’s situation and expectations of the seating intervention will also vary. Discussing these with the client is the key to determining realistic, appropriate seating goals. The goals of spinal seating are to determine a seating configuration that considers:
- Pressure management
- Postural support
- Functional capability, and
- Comfort.
Achieving a good seating result is often an involved and iterative process; initial trials typically yield additional previously hidden information that is relevant to the client’s seating and must be considered in the ongoing intervention. A key message of these modules is to appreciate the complexity of spinal seating and to not be disheartened if the process is not resolved quickly.
The process of achieving good results in spinal seating can be challenging and time intensive. The outcomes are extremely important as they affect major aspects of a client’s life. A client whose equipment is well selected and properly configured will typically have better healthcare outcomes, both directly and indirectly related to seating with lower risk of pressure injury, better supported posture, increased comfort and functional capability. Time invested to ensure that the correct equipment is selected and then configured appropriately will reduce the need for later intervention which is likely to be more complex and frustrating, both for the client and the therapist.
Spinal seating modules ‘roadmap’
The 10 modules in this series are intended to provide an introduction to the fundamentals of spinal seating and are arranged to reflect the various stages of systematic assessments and clinical interventions, from the initial client interview through to scripting an appropriate wheelchair.

- Introduction to the spinal seating modules
- Developing a client profile: Getting the big picture
- Hands-on assessment
- Body measurements
- Evaluation of client seating and wheel mobility equipment
- A framework for seating and mobility intervention
- Postural interventions
- Pressure management
- Manual wheelchairs and propulsion-assist devices
- Power wheelchairs
Systematic Assessment modules:
Module 2 discusses the process of meeting a client for the first time, developing a client profile and beginning to look at reasonable outcomes from a seating intervention.
Module 3 and Module 4 outline the process of assessing and recording details of the client’s body measurements and postural presentation. This information is critical for determining what strategies to pursue in an intervention.
Module 5 describes the process of reviewing the client’s existing equipment and determining its ongoing suitability.
Intervention Modules:
Module 6 presents a framework for seating interventions to help ensure a thorough, systematic approach.
Module 7 and Module 8 deal with posture and pressure respectively. These topics are typically the two most complex areas to manage with SCI clients.
Module 9 and Module 10 provide an overview of manual wheelchairs, propulsion-assist devices and power wheelchairs to help guide thinking when a client needs new or replacement equipment.
The Seating and Wheel Mobility (S&WM) Assessment Timeline below offers a chronological order of seating assessment and intervention tasks to be conducted from varies modules. It aims to minimise the number of client’s transfers and to improve time efficiency of the process.
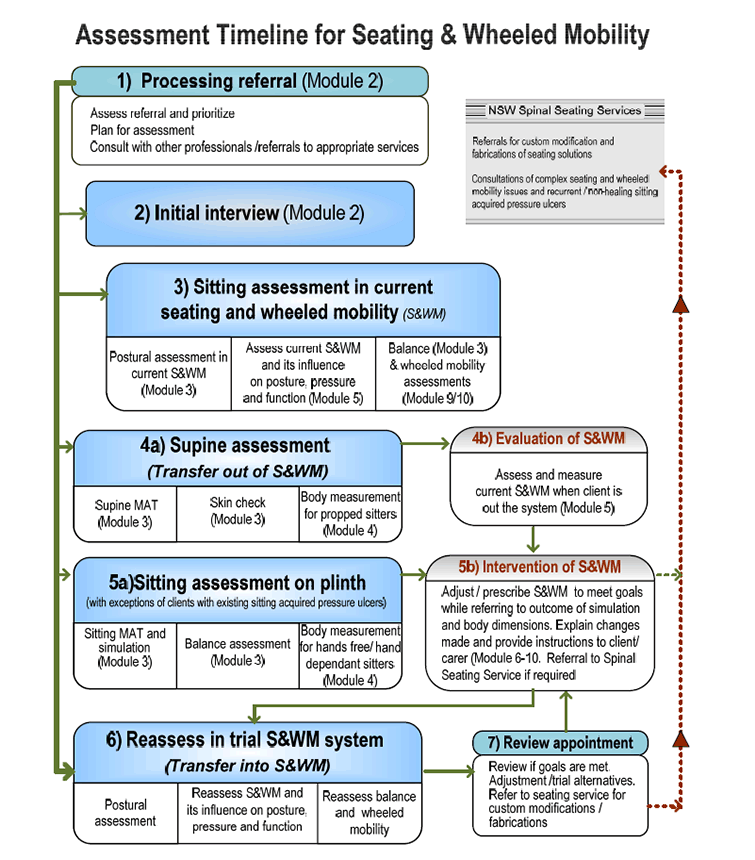
Assessment Timeline for Seating & Wheeled Mobility
- Processing referral (Module 2)
- Initial interview (Module 2)
- Sitting assessment in current seating and wheeled mobility
- Supine assessment
- Sitting assessment on plinth
- Reassess in trial S&WM system
- Review appointment
References
- WHO Fact Sheet #384. November 2013. Online article: accessed 11/03/2016. Available online at: http://www.who.int/mediacentre/factsheets/fs384/en/
- NSW Agency for Clinical Innovation, 2014. Model of care for prevention and integrated management of pressure injuries in people with spinal cord injury and spina bifida. NSW Agency for Clinical Innovation, March 2014. Accessed: 11/03/16. Available online at: http://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0005/214925/Spinal-Cord-Injury-Spina-Bifida-Model-of-Care.pdf