State Spinal Cord Injury Service
Spinal Seating Modules

Be systematic: Identifying pressure issues in seating
Seating related pressure risk or injuries are identified during the referral and interview process (see Module 2):
- Where is the pressure injury? When did it first occur? How frequently did it appear?
- What stage is each pressure injury?1
- Was the wound initially caused by incidents or trauma, such as a fall or mishap during transfer?
- What quality of sensation does the client have which may help protect against pressure injury?
- How many hours does the client generally sit in the wheelchair over a 24-hour period, and how many hours of sitting without weight-shifting or effective pressure relief?
- Is a change in the client’s ability to implement effective pressure relief a factor?
Further investigations are conducted through skin check, assessment of posture, balance and function (Module 3), body dimension (Module 4) and evaluation of current seating and mobility system (Module 5).
- Which area on the support surface corresponds with the placement of the injury on the body?
- Is postural asymmetry leading to uneven weight distribution a factor?
- Does postural instability lead to excessive uncontrolled movement in the seating system?
- Do performing functional tasks result in tissue damage?
- Are there problems with wheelchair and seating equipment not being appropriate to the client’s body ‘size’ and ‘shape’ and increasing the risk of pressure injury?
- Is the pressure management equipment properly maintained?
- Is equipment misuse, inadequacy, damage, breakage or wear a factor?
Setting pressure management goals in the client’s context
Prevention and management of pressure injuries should be:
- Client-centred: promoting self-management
- Comprehensive: covering the 24-hour pressure care needs of the individual
- Proactive: across the continuum of care
- Engaging: with multidisciplinary team and Spinal Seating Services.
When developing seating goals for pressure management, clinicians should consider the following:
- Consider posture: sitting posture can influence on the magnitude of pressure on each bony prominence is being loaded against the support surfaces. Postural intervention may lead to a reduced pressure in concerned areas, and pressure loads distribution may be taken with improved symmetry. Sitting posture should be well support to minimise shear (see Module 7)
- Select appropriate pressure care equipment individualised to the client’s body ‘size’ and ‘shape’
- Consider the components and features in the wheelchair and seating system that support and maintain the client’s functional ability to independently perform an effective weight-shift, and
- Ensure that pressure care products are correctly used and maintained by client or carer by providing adequate training of equipment usage.
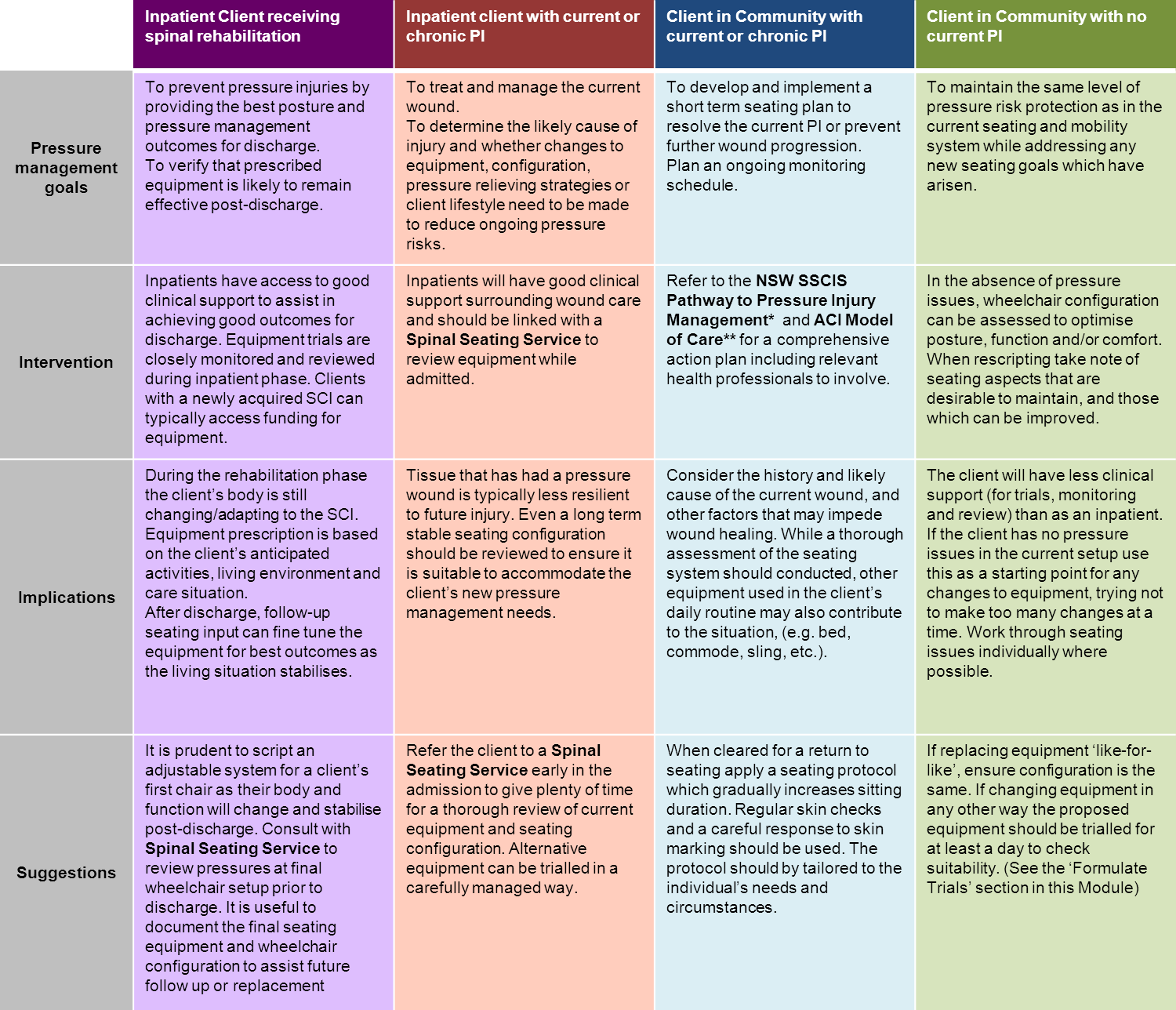
When setting the goals for pressure management consider the client’s stage in their journey through the continuum of care:
Figure 1: Goals for Pressure Care at various stages through the continuum of care.
*NSW SSCIS Pathway for Pressure Injury Management
**ACI Model of Care
References
- NSW Agency for Clinical Innovation. State Spinal Cord Injury Service Model of Care for Prevention and Integrated Management of Pressure Injuries in People with Spinal Cord Injury and Spina Bifida. Agency for Clinical Innovation, NSW: 2015.