Spinal Seating Modules

Gathering information for the client profile
The more information that is known prior to the clinical assessment, the easier it will be to plan an effective assessment. It is recommended that a comprehensive client profile be completed during the planning phase and at the initial assessment. Use the link below to download a form that can be used for recording client profile information.
Medical History and Physical Attributes
The client's medical condition relates to the clinical requirements of the seating and mobility system.
Primary and secondary diagnoses
Primary and secondary diagnoses reveal:
- Progressive vs. stable condition
- Acute vs. chronic condition
- Present and future needs.
- E.g. A client with a motor bike accident resulting in an L5 spinal cord injury, right scapula and humerus fractures uses powered mobility initially in the rehabilitation phase and then progresses to use a manual wheelchair
- The features on the wheelchair that match the clinical condition
- E.g. A client with an L5 complete spinal cord injury since 1960 has bilateral shoulder overuse syndrome and carpel tunnel syndrome and may need to progress from manual to powered mobility
- How often the wheelchair will be used
- E.g. A client with an L5 incomplete spinal cord injury walks with 1 crutch and uses a manual wheelchair for shopping only.
- Present and future needs.
Surgical history and considerations
Fractures and dislocations
Identify the causes, locations and the affect seating and posture. Some common examples are:
- Hip dislocation or fractured femur - leg length difference affects seat depth; detached femur encourages pelvic obliquity
- Fractured tibia/fibula - leg length difference determine footplate set-up
- Vertebra subluxations or fractures - fixed lordosis, kyphosis, scoliosis, cervical hyperextension or flexion
- Rib fractures - check spinal column for scoliosis instead of palpating rib cage. Take precaution when applying thoracic lateral support
Orthopaedic, surgical interventions and precautions
For example, shoulder conditions will alter the range of motion and strength for wheelchair propulsion. A client may lean to one side to compensate for weakness or restriction.
Orthotic/prosthetic device used
- Amputee - wheelchair set-up when prosthesis is on or off
- Spinal orthotic brace may determine seat angle and backrest options
- When did it happen/frequency?
- Where was the pressure injury?
- What was the wound grade?
- How did it occur?
- How was it managed?
Pressure injury history
- When did it happen/frequency?
- Where was the pressure injury?
- What was the wound stage?
- How did it occur?
- How was it managed?
Spasm
- Are there safety concerns due to spasm?
- E.g. A client’s foot slips off the footplate and drags along the ground after spasm.
- E.g. A client’s spasm pattern affects his control of the joystick.
- Are there postural and positioning concerns due to spasm?
- How does the client's tone or spasm affect their daily life?
- Is the client properly medically managed in these areas?
- Is the client partaking in drug trials that may influence seating outcome?
Sensation
Take into consideration the level of spinal cord injury, the completeness/incompleteness of the injury and the presence or absence of sensation. These will impact on pressure care management, hand function, balance, comfort and pain. Impaired sensation may increase the risk of secondary damage such as scrapes, burns and pressure injury. Impaired sensation may also make it difficult to achieve comfortable seating. It should be noted that sometimes impaired sensation does provide useful protective information, such as imminent risk of pressure injury, however the reliability of this sensation is individual.
Pain history
- A seating system may play a part in managing musculo-skeletal discomfort and pain. The following questions may help to establish if the pain is seating-related: When does it start/frequency?
- Where is the pain?
- What is the pain like (dull, burning, sharp etc.)?
- How did the pain occur?
- What triggers the onset of pain?
- What makes it worse?
- Client's perceptions of the cause, for example localised pressure, discomfort
- How is it managed?
- What has worked for the client as pain relief in the past, for example, bed rest, medication, change position/stretches?
- Is the client properly medically managed in these areas?
Cardiovascular, respiratory status and autonomic dysreflexia
- What are the implications of these conditions on the seating and mobility system?
- E.g. Seek information about exercise tolerance, endurance and oedema issues
- E.g. Are devices required for respiratory function, e.g. ventilator, BIPAP, CPAP?
- Is the client susceptible to autonomic dysreflexia?
Bowel and bladder function
- What is the current bowel and bladder management regime?
E.g. what aspects of the seating and mobility system will enable the client to perform transfers on the toilet or self-catheterisation in the wheelchair and to empty the leg bag?
- Does the client have a history of voiding difficulties when seated or recurrent bladder infections?
- How long does the client sit on the commode/toilet? (Pressure risk)
- Does the client have bowel or bladder incontinence? (Skin integrity risk)
- What continence aids are used? Where and when? (E.g. An incontinence pad or continence sheet over the pressure care cushion may protect the equipment but may also reduce the cushion’s effectiveness)
- Does the client have a supra-pubic catheter or ileostomy and if so does it conflict with the positioning of postural support equipment? (Pelvic belt may cause pressure over the catheter site)
- Consider the medical and nursing involvement, what potential considerations do these indicate?
Other medical conditions/physical attributes
- Adequate vision is required for safe independent mobility
- Hearing loss may require compensatory strategies for wheelchair training and independent mobility in the community environment
- Oromotor for speech and swallowing: is there a history of aspiration and low voice volume influenced by posture and positioning?
- Body weight: underweight and obesity contribute to a higher pressure risk. Client’s weight can influence product selection based on the weight capacity.
- Body height: impacts on equipment selection, based on size. Assess footplate/foot support clearance from the ground. Assess height clearance for tall clients when entering vehicles. See Module 4 for more information.
Psychosocial considerations
The following factors may influence seating and wheeled mobility selection:
- Cognition and ability to learn new skills, such as set up and maintenance of equipment, and the ability to adapt to new or changed equipment
- Visuospatial and perceptual skills
- Motor planning
- Communication skills, interpersonal and intrapersonal skills
- Judgement and safety awareness
- Behaviour and personality traits
- Motivation, attitude, acceptance of technology
- Self-image, the aesthetics and cosmetic preference towards wheeled mobility, and
- Co-morbidities such as mental illness and brain injury.
This information can be acquired through observations and input from the client and the client's health care providers. Refer to any psychological/neuropsychological reports when available.
Some clients with spinal cord injury may have comorbid mental illness and/or neurological changes such as brain injury and strokes. Consultation or referral to a medical practitioner, occupational therapist in neurology or psychologist may be indicated, particularly if there are safety concerns with independent wheeled mobility.
A social history and background will provide some guidance in setting realistic goals for seating intervention:

Socioeconomic circumstances
should be explored to maximize client's choice in equipment selection
- funding sources
- income status
- prospects of returning to work
- other funding schemes
- care packages
- known charities

Living arrangement and type of residence
- own home
- public or commercial rental
- residential care
- independent living units
- in group house

Family/carer support and its availability
- Ability to maintain equipment
- Hours of availability
- Key relationships
- Family dynamics

Cultural influence
on attitudes towards disability, carer's role and health care providers. Consider language barriers and the need to access interpreters and translated materials
Activities and participation
It is useful to ask the client to describe chronologically the activities involved in a regular day and on the weekend:
- How and where are they performed?
- What other equipment is used to participate in these activities?
- How often are they performed?
- How easy or difficult are they to perform in the current seating and wheeled mobility system?
Explore and discuss with the client the features of the seating and wheeled mobility required to carry out their activities of daily living. Record the discussion. Ask the client to demonstrate the activities or organise a site visit if needed.
Activities of Daily Living
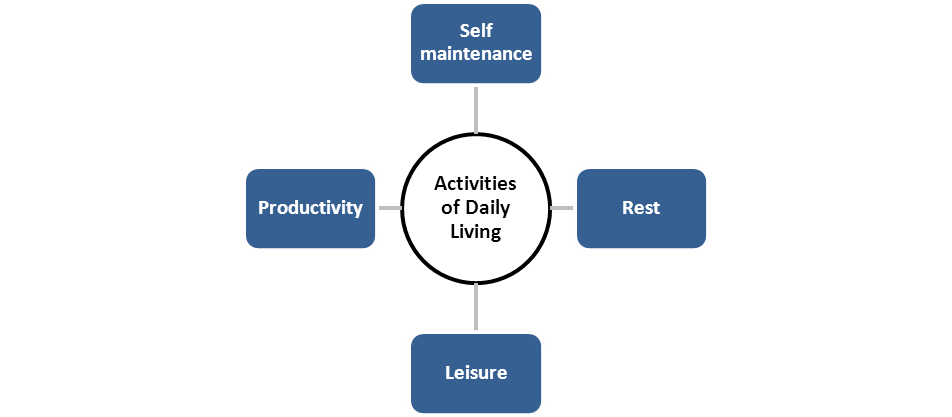
Self-maintenance | Personal care: toileting, showering, dressing Domestic tasks: meals preparation, cleaning, shopping Transfers: bed, chair, vehicle, commode, toilet Community mobility and transport: public / community transport utilized; is the client a driver / planning to drive a vehicle? State the type of vehicle and modification, method / equipment used by the client to stow/ secure the wheelchair in the vehicle. Consider dimensions required inside the vehicle when choosing a new wheelchair |
Productivity | Employment, education and training Carer duties Voluntary work Community participation |
Rest | Rest should be considered over a 24-hour period: in bed or wheelchair, use of seating functions such as tilt, or assistance required |
Leisure | Indoor, outdoor, terrains Climate, daytime, night time In confined, unpredictable, wet areas Special accessories or tools |
Environment
The environmental factors that will determine the features / specifications required in wheeled mobility include:
Internal home environment
- Indoor access: width of doorways, circulation space, kitchen bench and table heights, bathroom layout, floor surfaces
- Other residents or pets that would influence the selection of seating equipment.
External home environment
- Around the home: carport, clothesline, backyards
- Suburb of residence: flat or steep terrain, footpaths
- Terrain of frequent access: surface roughness, softness, slope and gradient
- Rural and remote areas: farm, dirt, gravel, thistles, burs
- Impact of climate on environment ie tropical, wet season, dry season, rainfall
- Temperature and moisture may influence the selection of material used for seating equipment
Work and leisure areas
- Access in office, workstations and work areas: clearance under desk/table
- Access to switches or control
- access to office areas and bathrooms
- Flat or steep terrain
- Parking
- Public transport route
Local community
Consider the accessibility and distances to:
- Local shops
- Medical or health centres
- Clubs, cafes or restaurants
- Parklands