Spinal Seating Modules
Recognise key relationships between the client and the wheelchair
Setting postural goals
A thorough assessment leads to appropriate goals; relevant goals lead to successful interventions.
There are usually many reasons for a specific postural presentation. Modules 2-5 will assist clinicians and clients to set clear clinical goals. A suggested strategy for setting postural goals is to consider the client’s ‘size’, ‘shape’ and ‘function’.
The client’s ‘shape’ (optimal sitting posture for balance, and skeletal alignment) was identified in Module 3 through flexibility testing and simulation. A review of the MAT outcomes will assist in setting postural goals.
The client’s ‘size’ was established through body measurement in Module 4 and compared with the existing seating system in Module 5. Review the dimensions recorded on the body measurement form and seating and wheeled mobility form to clarify goals related to size.
Review postural goals to see how these relate to the client’s functional capability. Discuss pros and cons with the client and, highlight compromises that may be needed. When considering postural intervention, pressure management should also be carefully considered as it may take a higher priority. The client may also wish to prioritise their functional capabilities over achieving a better posture.
Example
A client with T5 SCI presents with posterior pelvic tilt and thoracic kyphosis in his current manual wheelchair. Possible common causes for posterior pelvic tilt include:
- Fixed posterior pelvic tilt
- Fixed thoracic kyphosis against a planar back support, forcing the pelvis forward
- Tight hamstrings
- Seat depth is too long
- Foot plates are too low
- Inadequate postural support leading to compensatory posture to maintain stability and function
The list of possible causes is clarified by completing a systematic seating assessment as outlined in Modules 2-5:
The client has sufficient joint motion in the pelvis, thoracic spine, hip flexion and knee extension for the current wheelchair configuration when compared to the seating and wheelchair evaluation (Supine MAT). Possible causes 1, 2 & 3 identified above are eliminated.
The client’s thigh depth is longer by 40mm than seat depth when the pelvis is well positioned into the wheelchair (Body measurement, seating and wheelchair dimensions). The client’s lower leg length is well supported by footplates. Possible causes 4 & 5 are eliminated.
The client is a ‘hands-dependant sitter’. When arms are raised during the Sitting MAT, the client falls into a posterior pelvic tilt and thoracic kyphosis. During simulation, the client is able to erect trunk upright when the posterior superior iliac crests are supported. Support around the mid thoracic area enables the client to maintain lateral trunk stability while extending both his upper limbs for reach. The current wheelchair has a worn out fabric upholstery.
In this example, postural goals are established to provide adequate posterior pelvic support to stabilise pelvis and to provide lateral support at mid thoracic area to maintain trunk alignment for optimal function.
Keys to postural intervention
Postural stability
Posture is affected by the inter-related nature of the lower limbs, pelvis, trunk, upper limbs, head and neck. Postural stability facilitates optimal function and promotes safe and comfortable seating.
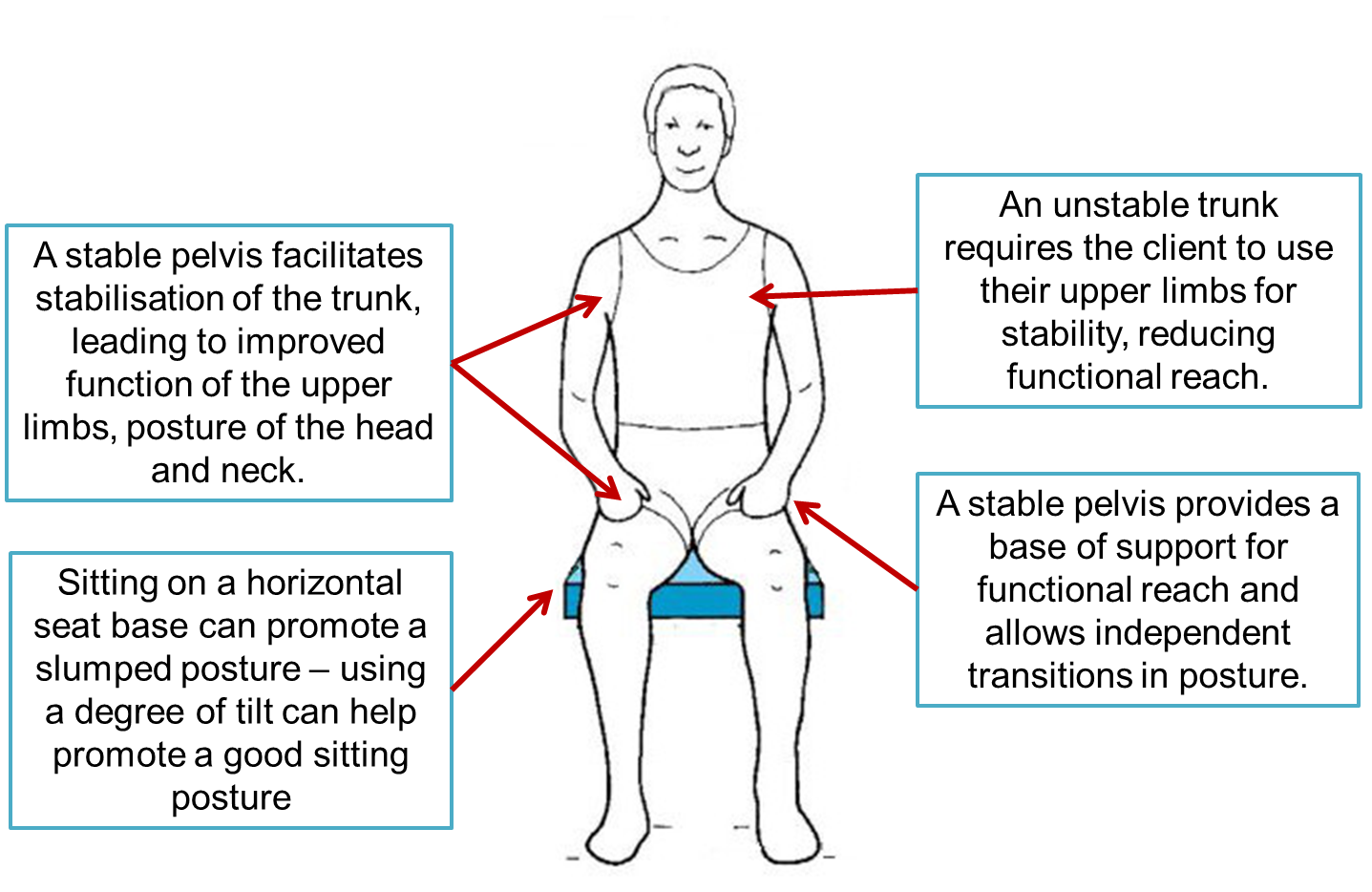
Figure 1: Examples of postural fundamentals.
Original image from Zollars1, modified by C. Turnbull, used with permission.
Depending on the client’s level of balance and function, wheelchair movements and uneven terrain will challenge stability if the client is inadequately supported. Therefore effective interventions will consider a range of postural controls to improve stability in various anatomical planes. Interventions for postural stability should support dynamic function and not reduce voluntary and functional movement (supports for transport requirements and safety concerns are an exception). Some postural supports may be contraindicated if there is a risk of injury (such as strangulation).
Material properties of support surfaces and covers, such as stiffness and friction, also influence postural stability.
Postural support and positioning
Body shape
A client’s body shape is an important consideration in seating. Body shape includes postural presentations, body mass distribution and the achievable ranges of motion in critical joints (hips, knees and spine). Accounting for the client’s body shape, the shape of equipment (including wheelchairs, armrests, legrests, headrests, backrests and cushions) should assist in achieving the four goals of seating.
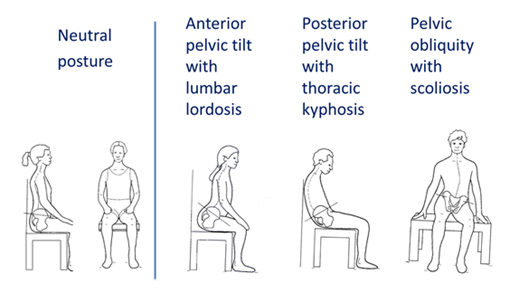
Figure 2: Common postural presentations.Original image from Zollars1, modified by C. Turnbull, used with permission.
Some practical considerations for seating with respect to the client’s body shape:
- Correct a flexible posture towards neutral, accommodate a fixed deformity to slow progression of the deformity2,3, partially correct and partially accommodate for ‘partially flexible deformity’
- Never correct posture beyond the range of motion established in the supine assessment.
- Consider all aspects of the mobility system when addressing postural issues. (Refer to Module 9 and Module 10), e.g. seat dump in MWC, and power seating in PWC.
- Match the sitting ‘angles’ in MAT evaluation to the seating system configuration to maximise postural alignment, stability and balance:
- Note the points of support needed during the sitting simulation
- ‘Seat support-to-back support’ angle should be adjusted to achieve the desired ‘thigh-to-trunk’ angle, and
- Consider the shape of spinal curves (the shape of supports required for lordosis and kyphosis and necessary seating angles).
- Configure or contour the seating system to compensate for body mass distribution and body build.
Example
- Clients with trunk and shoulders broader than their hips may require a wheelchair frame based on their upper body width. Hips guides or a contour cushion may then assist in centring the pelvis
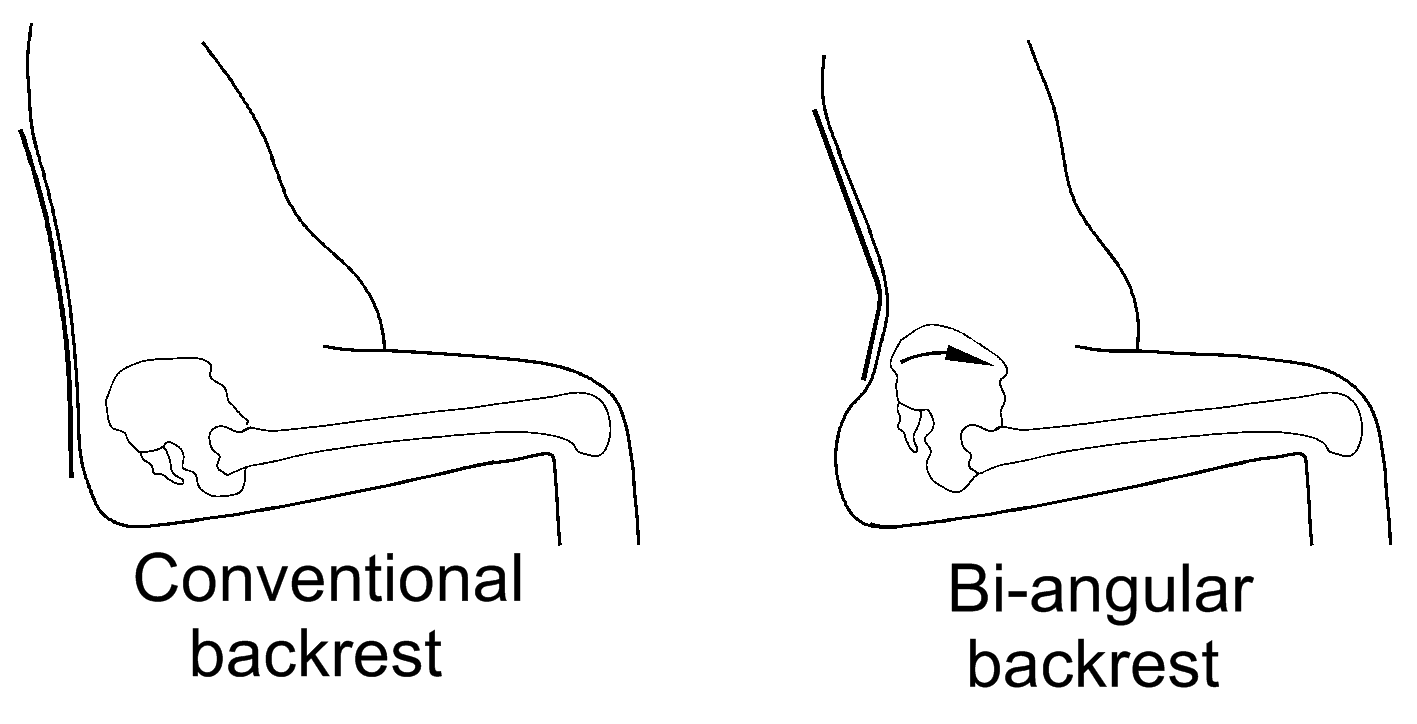
- Clients with a pronounce gluteal shelf may require a localised or bi-angular back support design so that the pelvis and spine are maintained in a neutral position.
- Customise postural equipment to support the desired client shape while maintaining functional freedom:
- Seat cushion design features may include an ischial well, modular or compartmental segments for correction or accommodation of pelvic tilt, obliquity or rotation. Pelvis and thigh stabilising accessories may be used.
- Back support designs can be described as planar, bi-angular, segmented or contoured. Many back supports have additional features to allow customisation: seat depth adjustment, seat to back angle adjustment, PSIS support, and built-in or additional thoracic lateral supports. When selecting a back support to meet the client’s needs, consider the effectiveness of the PSIS support and adjustment for lumbar and kyphotic curves, the height of posterior support required, the mounting position and depth of thoracic lateral supports. For supporting a scoliosis 3 points of control are most effective however this may unacceptably restrict the client’s function.
- When installing pelvic belts or upper body harnesses, assess for the ‘line of pull’ to optimise or correct body positioning.
- Other positioning accessories include anterior knee blocks and ankle huggers.
- Refer to a Spinal Seating Service for assistance for clients with severe postural deformity.
Body size
The client’s size is also an important consideration in seating. Body size includes overall height, width and girth, size of individual limbs including any complications with swelling including oedema. A client’s body size should be addressed by the shape and configuration of equipment (including wheelchairs, armrests, legrests, headrests, backrests and cushions) should assist in achieving the four goals of seating. Access and functional capability are two considerations that should be addressed specifically when considering body size.
Some practical considerations for seating with respect to the client’s body size:
- Ensure any proposed equipment can be configured or modified to adequately support and contain the client
- Allow the client to trial equipment at home and around their community to identify access or capability issues that will need to be addressed
- Recognise seating challenges associated with extreme body sizes, and how this may affect equipment choices. Be aware that it may be difficult to acquire trial equipment for extreme body sizes.
Incorrect size may lead to poor skeletal alignment, inadequate support and development of pressure areas and/or a compensatory posture in order to function. Refer to Module 4 and Module 5.
References
- Zollars, J.A., (Illus. Knezevich, J.), 1996. Special seating: An illustrated guide. Otto Bock Orthopaedic Indus., Inc., pp120.
- Negrini et al.: 2011 SOSORT guidelines: Orthopaedic and Rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 2012 7:3
- Hastings, Jennifer D., et al., 2014. "Conservative Treatment of Neuromuscular Scoliosis in Adult Tetraplegia: A Case Report." Archives of physical medicine and rehabilitation 95.12 (2014): 2491-2495.
https://pubmed.ncbi.nlm.nih.gov/24814562 - Wheelchair Provision for Children and Adults with Neuromuscular Conditions in British Columbia, April 2014
- Queensland Spinal Cord Injuries Service, accessed 2016.