Three common and effective approaches to providing chronic wound management services with virtual care that are used within NSW Health services include:
This list is not exhaustive of all service approaches using virtual care.
Hybrid chronic wound management services
A hybrid model involves chronic wound management care being provided both in-person and virtually as part of the same service offering.
Hybrid models offer a way for existing chronic wound management services to adapt and grow using technology, as consumers become more familiar and comfortable with virtual care.
Features of hybrid models
- The consumer can choose to access in-person or virtual care services, including a combination of both options, based on their need, preference and clinical suitability.
- Clinical documentation processes and other systems are shared across in-person and virtual care service delivery.
- A clinician can use virtual care technology to provide care directly to a consumer or to a consumer and another service provider. This can improve integration and coordination of care between services.
- Services should measure the consumer experience and outcomes, e.g. with patient reported measures. Differences in the consumer experience between types of service delivery should be monitored and explored.
Service examples
Murrumbidgee Local Health District (MLHD) and Southern New South Wales Local Health District (SNSWLHD) are two of the NSW Health services that have adopted a hybrid model of in-person and virtual care chronic wound management.
Virtual care services have reduced the need for consumers to travel long distances, improved access to specialist chronic wound management clinicians and built the wound management confidence and capacity of clinical staff accessing the virtual care services.
MLHD has extended its clinical nurse consultant (CNC) wound and stoma management services to incorporate virtual care approaches. This has improved service reach across the 125,000km² region. Services are provided as part of a hybrid model of care including virtual and in-person care.
Virtual care wound management services
- Responding to inpatient consultation requests via MedSync for sharing wound images, reviewing digital documentation and making phone calls
- Providing videoconference reviews with consumers with stomas at MLHD facilities. The consumer is set up with the videoconference equipment at their local health facility and the stoma management CNC dials in to engage in a virtual care review
- Providing CNC consultations and advice to community nursing services. Staff use a combination of videoconference, wound photography, text and phone calls to collaborate for a consumer's wound management
- Collaborating with Hospital in the Home virtual services to link consumers with appropriate wound management services
- Providing consultations to residential aged care facilities through wound photography sharing and phone calls
- Delivering short, regular videoconference education sessions to staff at multiple facilities before handover

SNSWLHD has 16 health service sites across its region, with five having onsite access to a wound management specialist. All sites have access to virtual care modalities and are using these to improve access and the quality of care that consumers with chronic wounds receive.
In addition to significant in-person services, the SNSWLHD community nursing CNC service provides chronic wound management services virtually.

Virtual care wound management services
- Providing CNC virtual care video consultations to other SNSWLHD sites where the consumer and their usual care team are present
- Participating in video consultations with consumers and their specialist burns and spinal unit services in Sydney and phone and digital documentation sharing with other tertiary services in Canberra
- Participating in videoconference case conferences with consumers, carers and the wider multi-disciplinary team
- Using wound photography store and forward platforms to share images and management advice between consumers, community health, general practice, non-government organisations, the National Disability Insurance Scheme (NDIS), Department of Veteran Affairs and specialist services
- Holding weekly virtual care videoconference huddles with staff from all SNSWLHD sites to review and discuss consumers with challenging chronic wound management needs. Staff can share wound photos and digital documentation with the CNCs and other colleagues in real time to inform advice an d management options
- Providing staff education over video conference and uploading the recordings to the SNSWLHD My Health Learning and Teams channels for staff to review at any time.
Specialist chronic wound management virtual care services
Specialist chronic wound management virtual care services are those developed specifically to connect clinicians who are skilled in chronic wound management with consumers and other care providers. Services are mostly provided via virtual care but may include some in-person elements.
The chronic wound management specialists are often registered nurses trained in wound management (including clinical nurse specialists (CNSs), clinical nurse consultants (CNCs) and nurse practitioners) and may also include medical and allied health team members.
The specialist chronic wound management virtual care services provide care directly to consumers or offer specialist support and advice to other clinical services. They use a range of virtual care modalities.
Services delivered
- Wound management virtual consultation to the consumer and their care team. This could be to care teams on an inpatient ward, in community health, outpatient clinics, residential aged care facilities, primary care services, in the home or other care settings. Consultation may involve assessment, determination of wound aetiology, goal setting, development of a management plan, supervision of treatment, review of progress and discharge planning.
- Direct engagement with the consumer and their carers for their chronic wound management. This could include providing advice or supervision for self-management, information and education or review of wound progress. These services can be delivered via a range of virtual care modalities, including virtual consultation, wound photography with image sharing and messaging.
- Participating in video case conferencing and discharge planning.
- Offering specialist advice to other clinicians via a range of virtual care modalities.
- Providing a virtual care rapid response service to emergency or hospital avoidance services.
- Providing remote patient monitoring services with consumers and their care team.
- Offering virtual wound management clinical education to healthcare staff.
“The virtual service has taught me so much about my health and why this wound would not heal.”
“I felt power to take control of my life, so one day I could return back to work, and even back to the community and without their help I know I wouldn’t have been able to do that.”
“I can really feel a huge difference that the wound centre has provided me.”
WNSWLHD Virtual Wound Management consumers
Service examples
The Western New South Wales Local Health District (WNSWLHD) Virtual Wound Consultancy Service has been providing nurse-led specialist wound management advice to rural and remote health services across the region since commencing in 2018.
Access to service
All WNSWLHD acute, community and aged care services can access the service by:
- completing a referral form
- providing multiple photographs of the wound
- emailing the information to the service.
The Virtual Wound Consultancy Service is staffed by a CNC. Referrals are triaged by the CNC and actioned in response to their category.
Priorities for treatment
- Chronic wounds with localised or treated infections
- Palliative wounds
- Stage 3 and 4 pressure injuries
- Wounds that are deteriorating
- Wounds that are not improving or are non-healing
- Other chronic wounds requiring investigation and review
Wounds requiring urgent medical review or wounds out of scope of the service, e.g. acute wounds, diabetic foot ulcers and stage 1 and 2 pressure injuries, are referred to other services.
Consultations
The CNC will undertake an extensive documentation review before meeting virtually with the consumer and their care team.
The consultations occur over videoconference at a WNSWLHD health facility with the consumer and a healthcare worker, e.g. a community nurse, Aboriginal health practitioner or aged care worker, together in the room.

Part of the initial consultation will involve ensuring the environment is suitable for a virtual consultation.
During consultations the CNC will:
- validate information provided
- ask new questions of the consumer and healthcare worker
- observe the wound with video
- complete diagnostic investigations supported by the healthcare worker in the room, e.g. a Doppler ankle brachial pressure index for lower limb wounds.
- explore the consumer’s management goals
- develop a management plan and treatment regime
- support the healthcare worker to perform the wound treatment on the day, e.g. guidance for applying compression or other wound management products.
Ongoing support
The Virtual Wound Consultancy Service provides review appointments, case conferencing, referral, and advice to colleagues. The service is building the knowledge, confidence and skills of consumers and staff with the aim of improving chronic wound management capability across WNSWLHD.
Sydney Local Health District (SLHD) is at the forefront of adopting virtual consultations as part of the management of chronic wounds.
The RPA Virtual Hospital Wound Care Command Centre was established with the vision:
“To ensure that every individual with a chronic wound has timely access to wound care”.
Their goal is to ensure that every individual, no matter where they are, receives the best possible treatment and support for their wound.
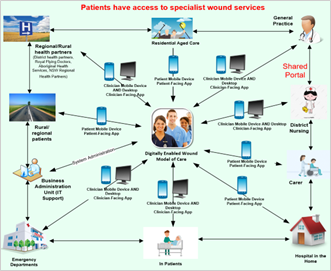
The Wound Care Command Centre provides a nurse-led service. The service uses an artificial intelligence digital wound application called Tissue Analytics to connect individuals, their family and carers, hospitals, specialist services, community care, and residential care to specialised wound management and expert advice and enhance shared care.
Access to service
Consumers living with a chronic wound are eligible to access the Wound Care Command Centre if:
- they are 18 years of age or older (people 16 and 17 years of age are considered on a case-by-case basis)
- they have a wound that has not healed within 30 days
- have other risk factors complicating healing, e.g. co-morbidities, infection, and excess exudate.
The service also provides post-discharge follow-up for hospital-acquired stage 3, 4 and unstaged pressure injuries, and suspected deep tissue injuries.
Referrals are accepted from acute and rehabilitation hospitals, emergency departments, hospital in the home, Sydney District Nursing, general practitioners, residential aged care facilities, rural and regional partners, and directly by individuals with wounds, their family or carer.
Referrals are triaged by the co-ordinating transitional nurse practitioner (TNP), with clinical support from CNCs and a CNS.
Tissue Analytics App
The Tissue Analytics app enables individuals to capture photos of their wounds and securely communicate with healthcare practitioners at the Wound Care Command Centre for remote monitoring, analysis, and ongoing care. Clinicians benefit from advanced 2D and 3D imaging wound analytics, diagnostics, clinical decision formulary and error-free tracking and documentation.
Consultations
When a consumer is accepted into the service, an initial consultation is conducted in-person at the RPA HealthOne Green Square wound clinic, at a SLHD hospital, residential aged care facility or at the consumer’s home.
The initial consult allows the nursing team to assess the wound in-person and enables the team and individual with the wound to download Tissue Analytics to their smart phone device (if they do not have a device, SLHD will provide one).
Ongoing support
Wound treatment and advice are continued via the Wound Care Command Centre remotely using telephone, videoconferencing, and the Tissue Analytics app.
Ongoing wound dressings or other treatments may be provided by the consumer’s primary care team, residential aged care facility staff, community health nursing or self-managed with support of the Wound Care Command Centre.
Other virtual care services providing some chronic wound management
Other virtual care services can play a role in providing some chronic wound management, especially identifying consumers with unmanaged chronic wounds, providing interim care solutions, and connecting consumers to ongoing chronic wound management services. These services include:
- Hospital avoidance services
- Hospital in the home
- Other integrated care services
Services delivered
- Screening consumers to identify those at risk of developing a wound or with unidentified or unmanaged chronic wounds.
- Referring and connecting consumers to appropriate chronic wound management services, including community health and primary care.
- Troubleshooting and support for self-care for consumers until they can access a chronic wound management service.
- Offering remote monitoring or Hospital in the Home services for people with specific wound needs, e.g. virtual care pathways for people experiencing cellulitis.
Service example
Since 2021, the Mid North Coast (MNC) Virtual Care service has developed and evolved, expanding the clinical conditions that can be managed safely in a virtual space. As the service grows, MNC Virtual Care is providing more wound management services, including interventions to prevent acute wounds from progressing to chronic wounds.
Access to service
Services are provided to suitable patients within the Mid North Coast Local Health District (MNCLHD) at risk of presentation to hospital or requiring early supported discharge from hospital. The MNC Virtual Care clinical team is made up of medical officers and nurses.
Virtual care wound management services provided
- Pathway for outpatient management of cellulitis for people who have been prescribed oral antibiotic treatment.
- Supporting consumers or their carer to self-manage existing wounds.
- Reviewing healing of surgical wounds.
- Connecting consumers with appropriate ongoing wound management services.
Consultations
The MNC Virtual Care clinical team makes first contact with the consumer by telephone call, often converting this call to a video call using a smart phone or tablet, using the myVirtual Care teleconferencing platform. This enables the team to visually review the cellulitis and any wounds that may be present.
For smaller wounds, the consumer is encouraged to take photographs of their wound and email them to the clinical team so they can take a closer look at the wound features and monitor healing progression over time. These photos are uploaded to MedSync and saved in the consumer’s medical record.
The MNC Virtual Care team also provides flexible wound management services in response to consumer needs. This includes following up wound swab results and adjusting medications as required, supporting consumers or their carer to self-manage wounds, reviewing wound healing, and connecting consumers with appropriate ongoing wound management services.
The nurses support the consumer with self-management of the wound, using a video call to:
- review and assess the wound
- guide the consumer in wound care, including cleaning the wound, dressing choice and application
- provide education on wound healing.
- monitor for signs of wound deterioration with established clinical emergency response system protocols in place for patient deterioration and escalation.