Thank you to the clinicians, health managers, consumers and stakeholders who work with us to drive healthcare innovations across NSW.
Clinical network and taskforce updates
More than 300 clinicians and researchers came together at the Australian & New Zealand Burn Association Annual Scientific Meeting at Luna Park, on 13-16 September 2022. The event included a dinner celebrating people working in burn injury with the theme ‘Everyone is a Superhero’. The Burn Injury Network contributed to organising and hosting the event.
Panel discussions throughout the event were well received and sparked further discussion about the improvement of burn disaster preparedness and dermal replacement.
Awards were presented for burn care, prevention, research and education. Congratulations to the following NSW Statewide Burn Injury Service members who received awards:
- Highly commended for burn care, oral presentation: Miranda Pye, Nurse Practitioner, Concord Repatriation General Hospital
- Winning burn care, ePoster: Julie Bricknell, Physical Therapy, Royal North Shore Hospital
- Winning burns prevention, oral presentation: Siobhan Connolly, Education and Prevention Officer, Agency for Clinical Innovation
- Winning burns prevention, ePoster: Dinuksha De Silva, Junior Medical Officer, Royal North Shore Hospital
- Highly commended burns research, oral presentation: Kevin Tsai, Researcher, The ANZAC Research Institute at Concord Repatriation General Hospital
- Winning burns education, ePoster: Anne Darton, Network Manager, Agency for Clinical Innovation
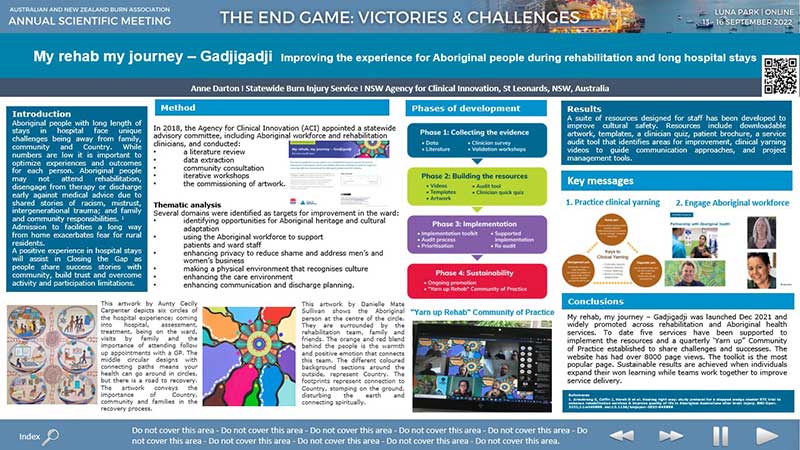
Winning burns education ePoster, My rehab, my journey – Gadjigadji.
Learn more or contact the Burn Injury Network.
The network would like to acknowledge and thank Professor Greg Fulcher, who has completed a three-year term as Medical Co-Chair.
Professor Fulcher, along with co-chairs Elizabeth Obersteller and Irene Kopp, led the network’s involvement in two Leading Better Value Care initiatives and contributed to other network-driven projects.
As clinical lead of the Diabetes COVID-19 Community of Practice, Professor Fulcher also led the network’s response to the pandemic, including the development of vital resources and guidance documents.
Professor Fulcher remains a valuable network member, currently sitting on several working groups.
The network welcomes Professor N Wah Cheung as the new Medical Co-Chair. Professor Cheung is the Director of Diabetes and Endocrinology at Westmead Hospital, Western Sydney Local Health District.

Professor Greg Fulcher

Professor N Wah Cheung
Learn more or contact the Diabetes and Endocrine Network.
The taskforce has published new progressive resistance training for frailty resources to support physiotherapists and exercise physiologists prescribe and provide progressive resistance training (PRT) to older people living with, or at risk of, frailty.
The evidence-based resources include:
- video demonstrations of specific exercises
- videos that share the benefits of PRT
- a guide for health professionals
- the truth about PRT for consumers and clinicians.
A group people in their eighties and nineties who do PRT regularly demonstrate the exercises. They are guided by expert clinicians and share the benefits of this type of training.
This project was led by Professor Maria Fiatarone Singh who is a geriatrician and Bev Gow-Wilson, the Agency for Clinical Innovation’s Primary, Integrated and Community Health Network Manager. Learn more about the project in this issue of Clinician Connect.

Dr Nathan de Vos guides Sylvia through an exercise.
Learn more or contact the Frailty Taskforce.
Congratulations to Professor James Middleton, the service’s Co-Chair and Clinical Director, who has received the prestigious International Spinal Cord Society Annual Medal for 2022.
Known as the ‘society medal’, it is awarded each year to someone who has made an outstanding contribution to spinal cord injury (SCI) prevention, treatment and research.
Professor Middleton will join an international group of dedicated SCI pioneers who have received the award since 1976, recognising his tireless dedication to enhancing treatment and quality of life for people with SCI.
Learn more or contact the State Spinal Cord Injury Service.
Congratulations to the Rural Stroke Coordinators Community of Practice for presenting at the recent Smart Strokes Conference. Fiona Ryan, the Stroke Care Coordinator for Bathurst and Orange, presented on behalf of the group and spoke about:
- the Realising Improvement in StrokE (RISE) program
- establishing a process to facilitate benchmarking and quality improvement in rural stroke care.
The RISE program is now available to all NSW hospitals.
Learn more or contact the Stroke Network.
The taskforce is pleased to welcome Professor Neil Merrett to the role of Chair. Professor Merrett is the Program Director of Surgery at South Western Sydney Local Health District and Foundation Professor of Surgery at Western Sydney University and the University of NSW.
As a member of the taskforce for more than 10 years, Professor Merrett has been instrumental in:
- developing value-based surgery and enhanced recovery after surgery principles
- surgical optimisation efforts
- state-level policy for planned and emergency surgery.
Professor Merrett is also an active member of the Surgery Community of Practice and Clinical Council, contributing to the health system’s COVID-19 response and recovery efforts.
The taskforce thanks and farewells Professor Arthur Richardson for his leadership as Chair over the past seven years, and in the Surgery Community of Practice since 2020.
Professor Richardson’s achievements include:
- driving significant changes in surgical services design
- developing innovative models of care
- leading implementation of the National Surgical Quality Improvement Program in Australia.
Professor Richardson will continue to advocate for quality, safety, and professionalism in surgical care. His dedication and sense of humour will be missed by the network.

Professor Neil Merrett

Professor Arthur Richardson
Learn more or contact the Surgical Services Taskforce.
Key principles for transition
The network has launched its updated key principles for transition in a new digital format. The resource provides advice, templates, resources and examples for clinicians and services to support young people with a chronic condition or disability as they move from paediatric to adult health services.
Thank you to everyone who contributed to the update and provided feedback.
Over the coming months and year, the network will focus on supporting implementation of the principles.
Share your experiences of transition care
To complement the network’s recently completed consumer survey and meetings with local health districts, we are seeking insights and advice from clinicians and health services about experiences of providing transition care.
Please complete this survey and share among your colleagues, services and clinics. Your feedback will inform future network priorities and projects.
Learn more or contact the Transition Care Network.
The stream hosted the 7th National Disability Insurance Scheme (NDIS) virtual community of practice event on 20 September 2022.
More than 280 clinicians attended from across NSW to learn about hospital discharge delays for NDIS participants, presented by Sarah Morton, Director of Disability, Youth and Paediatric Health from the Ministry of Health.
Attendees also learnt about recent and upcoming changes to the NDIS and enjoyed the opportunity to ask questions of the Ministry of Health’s disability team.
Statewide program updates
Our Renal, Musculoskeletal and Diabetes and Endocrine Networks are part of the Leading Better Value Care (LBVC) electronic medical record (eMR) project. The project is a collaboration with eHealth NSW and the Ministry of Health, clinicians and health managers. The project started in early 2020 to design, build, implement and evaluate eMR tools to support these LBVC initiatives:
- osteoporotic refracture prevention
- osteoarthritis chronic care program
- renal supportive care
- inpatient management of diabetes mellitus.
Thank you to network members for the vital clinical engagement you provided and your significant contributions to the eMR solutions developed by eHealth NSW.
Throughout the COVID-19 pandemic, network members continued to participate in eMR design and implementation working groups, beta and user acceptance testing, piloting and evaluation. This dedication to person-centred innovation ensured that strong leadership and advocacy for practical and effective eMR solutions were central to the project.
Learn more about Leading Better Value Care.
Positive consumer feedback
Virtual care gives patients more options to access healthcare. Last financial year, more than 220,000 consultations were held on the myVirtualCare platform, with patients reporting* very positive experiences.
Of the 25,700 survey responses:
- 96% said the virtual care they received was good or very good
- 96% said their health professional explained things in a way they could understand
- 94% said their health professional listened carefully to views and concerns they had
- 79% said their virtual care experience was better or the same as an in-person appointment
- 81% said they didn’t experience problems with their connection or technology.
Patients surveyed said:
- “I was very impressed with the service today”
- “The nurse was calm and reassuring…”
- “Quite happy with the appointment and results”
A small number of survey respondents identified the following challenges for virtual care:
- trouble hearing the health professional
- technical difficulties
- some healthcare being better suited to in-person appointments (such as physiotherapy).
These valuable insights will help inform improvements in virtual care delivery.
*Patients using myVirtualCare were surveyed between July 2021 and March 2022. More than 25,700 surveys were received across 15 local health districts and two specialty health networks.
Virtual Care Central reaches 100,000 site visits
Virtual Care Central has reached the significant milestone of 100,000 site visits.
The site is a central hub of virtual care information, resources and news for NSW Health staff. It can also help you identify and connect with colleagues who can support integrating virtual care into your clinical practice.
The site will soon be reviewed to ensure it is meeting user’s expectations. To be involved, please email aci-virtualcare@health.nsw.gov.au
Virtual Care Central.
New resources available
The following new or updated resources have been developed to support clinical teams delivering virtual care. They are available on Virtual Care Central.
- Pexip – A guide to delivering group sessions
- Guidance for virtual care hardware
- Frequently asked questions
For consumers, the Technical issues – troubleshooting guide is also available on the ACI website.
myVirtualCare user guide and training milestones
The myVirtualCare online user guide has received more than 10,000 visits since launching in February 2022. The user-friendly guide allows clinicians and consumers to quickly search for myVirtualCare tips and information.

myVirtualCare online user guide.
myVirtualCare training courses are also available for NSW Health staff. The training is offered in a variety of ways to suit learning preferences and availability. Staff have completed more than 12,000 training modules so far.
Learn more about virtual care and the training on offer on Virtual Care Central.