Read the latest updates on the people involved and progress made across the ACI’s clinical networks, institutes and taskforces.
- In September 2020, the Patient Special Project (PSP) was established through a collaboration between the Aged Health Network, the Clinical Excellence Commission, University of Wollongong and clinical nurse representatives from local health districts. The PSP aims to improve the care and management of patients who require supervision and interventions to remain safe while in hospital. This involves developing a key principles document and clinical toolkit. A number of activities have been underway to inform this work.
- The ACI’s Evidence team assisted in sourcing data to support the direction of the work. This was a difficult task given there is no standardised term used when providing a patient special service.
- Working with the NSW Health Nursing and Midwifery Office the PSP team distributed a survey to staff seeking information about their local patient special services. A total of 434 surveys were returned; many suggesting that improvements to system processes and workforce education and training were required.
- The PSP team were invited to present at the State Directors of Nursing and Midwifery meeting in April. It was a fabulous opportunity to engage with the group and consult on the direction of the work.
- The Clinical Excellence Committee’s Patient Safety Unit isolated a total of 1,239 incidents by using search terms relating to ‘patient special services’ between 1 January and 25 April 2021. The data identified patients as having high risk of falls, cognitive impairment, confusion, dementia, delirium or mental health history.
- The PSP team held two workshops with NSW clinicians and managers in May 2021, to discuss issues related to patient special services. One in-person workshop was held and the other was held virtually to reach staff who could not travel to Sydney. Both workshops were a success in brainstorming issues, solutions and building the foundation of a key principles document and clinical toolkit.
We are saying goodbye to Justine Watkins, Manager of the Aged Health Network and Deb Moss, Project Officer at the end of June 2021. They have successfully engaged health staff to participate and move the project forward to ensure the outcomes of the PSP match the needs of the clinical community.
Glen Pang will return as manager of the Aged Health Network from 1 July 2021 and looks forward to moving forward with the PSP and other network activities.
Find out more and contact the Aged Health Network.
June is National Burn Awareness month, a joint initiative between Kidsafe and the Australia and New Zealand Burn Association. It aims to drive greater awareness of prevention and correct first aid treatment for burns.
The ACI Statewide Burn Injury Service (SBIS) is the largest burn service in the country and is actively involved in promoting prevention and first aid messages to the NSW community. Recently, we spoke to ABC Radio Sydney’s Focus program about the prevention of microwave-related burns. Anne Darton, SBIS Manager, talked about specific dangers and cautions with the use of microwaves and burn injuries.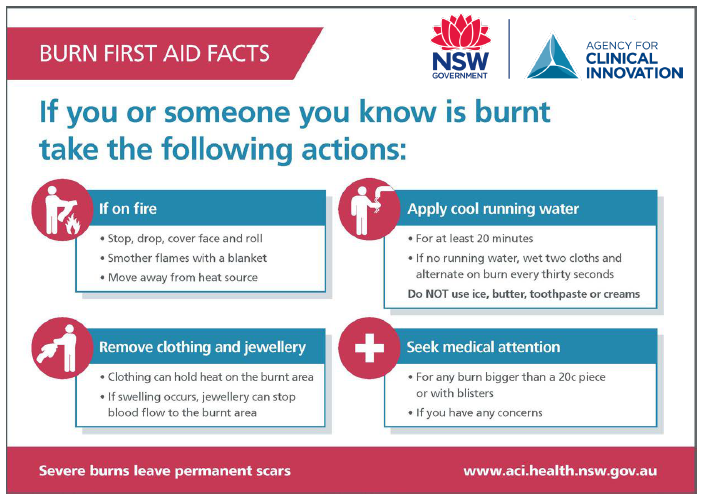
Burn first aid facts.
Find out more and contact the Burn Injury Network.
The new Clinical Principles for End of Life and Palliative Care will soon be available. The guideline outlines the clinical principles and key actions that support good quality, evidence-informed practice and improvement in end of life and palliative care in NSW. It applies to all care settings and people across their lifespan. NSW Health services should use the guideline to inform local models of care to ensure that community needs are met. More information and materials to support local implementation will be shared in the coming months.
A self-assessment tool is also being developed to provide NSW Health services with an instrument to analyse their current performance, capacity and support requirements to implement the guideline and key actions.
A consumer resource to accompany the guideline will also be developed.
Find out more and contact the End of Life and Palliative Care Network.
The Mid North Coast Local Health District will be the first trauma network to undertake the NSW Trauma Verification Program over the next few months, including the trauma services of Coffs Harbour and Port Macquarie. The Hunter New England Local Health District will follow.
Read more about this in our feature story.
The Pain Management Network sponsored a workshop in Orange to provide general practitioners, junior doctors and other health professionals with updated evidence on cannabis and opioids, and an insight into the impact of current guidelines on the prescription of both medications.
The workshop was hosted by the Orange Chronic Pain and Rehabilitation Service. Dr Steve Gibson, Anaesthetist and Pain Specialist at Royal Prince Alfred Hospital, was the guest speaker.
The workshop also provided an opportunity to observe a musculoskeletal examination of the lower back and hip.
A total of 24 participants attended the event, either in person or virtually. Feedback on the event was positive.
Find out more and contact the Pain Management Network.
On 25 May 2021, the Rehabilitation Network hosted a workshop for clinicians, Addressing sexuality for people living with chronic disease. Presented by Dr Margaret McGrath (University of Sydney) and Sandra Lever (Northern Sydney Local Health District) from the Sydney Sexuality Group at Ryde Hospital, the workshop was attended by 25 clinicians from a variety of disciplines and specialty areas.
The workshop was designed to increase the knowledge, confidence and foundational skills of health professionals in providing sexual rehabilitation for people living with chronic disease. Starting the conversation is often the hardest part, and attendees report that they now feel more confident and comfortable in having these conversations with patients.
Find out more and contact the Rehabilitation Network.
The renal supportive care community, comprised of consumers and clinicians, have developed a survey to capture the experiences of carers, where they play a major role in the patient care team, across a variety of clinical specialities.
A total of 40 feedback forms have been received from a range of specialties. In addition to renal supportive care, these include frailty, mental health, heart failure, dementia, drugs and alcohol, disability, aged care, brain injury and palliative care.
Based on this feedback, an amended version of the Carer Reported Experience Measures (CREMs) survey will soon be piloted at several sites.
Any sites interested in piloting the updated CREMs survey can contact the Renal Network.
Find out more and contact the Renal Network.
Rural Innovations Changing Healthcare Forum
The 8th Rural Innovation Changing Healthcare Forum (RICH) was held on 24 March 2021.
The theme was 'rural health bounding forwards' – showcasing how service providers, consumers, communities and other sectors have embraced hope, strength and connectivity; and moved forward from hardships imposed by droughts, bushfires and the pandemic.
Network members can access the Rural Health Network SharePoint site page for presentations and the RICH 2021 evaluation report.
Improving the Rural Patient Journey Initiative
The refreshed Friendly Faces Helping Hands (FFHH) website contains information on 38 major metropolitan and rural referral hospital services. The aim is to help patients and their families navigate city services when healthcare is required away from home, kin and country.
As part of the ACI Aboriginal 8 Ways of Learning (A8WOL) program, an Aboriginal co-design group has been convened to review the FFHH website content, resources and promotional material for Aboriginal communities and organisations. An Aboriginal artist was commissioned in May to work with the group to develop resources.
Implementation of the FFHH website and resources will be fast-tracked from July onwards, to promote and embed FFHH across local health districts, NSW Ambulance, consumer groups, NSW Rural Doctors Network and Aboriginal organisations.
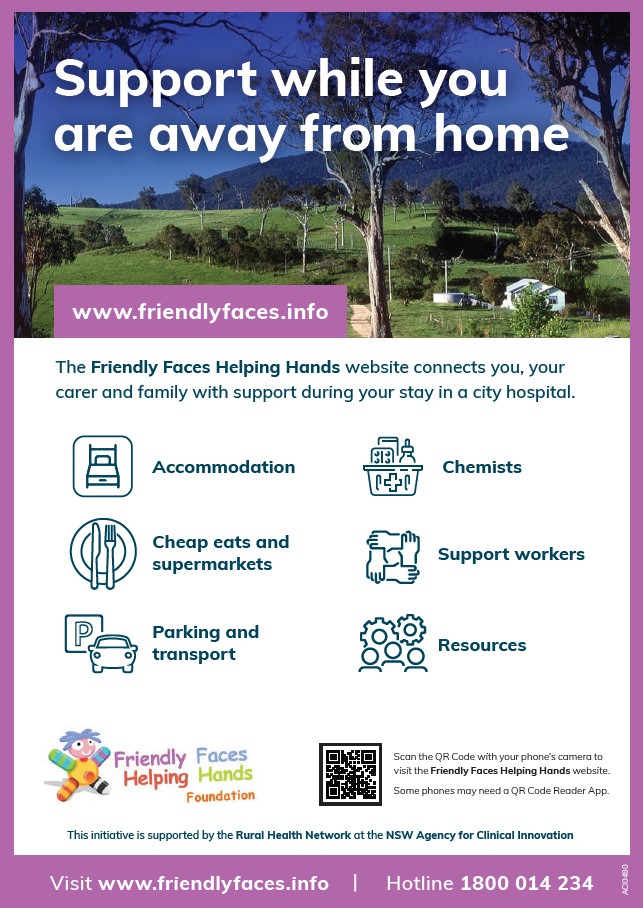
Friendly Faces Helping Hands flyer.
Rural Local Health District Health Awards and ACI Innovation Awards
As part of the 8th annual Rural Local Health District Health Awards and ACI Innovation Awards, the Rural Health Network will award a rural team who has addressed an issue of using existing resources, embedded the change and for the potential of transferability and sustainability.
The awards will run from June to August 2021.
Personnel updates
Two positions are available on the Rural Health Network Executive for a term of up to five years:
- Aboriginal consumer representative
- Aboriginal medical service representative.
Find out more and contact the Rural Health Network.
Trapeze and the ACI Transition Care Service supports adolescents to transition to adult healthcare services. We have recently reviewed our transition fact sheets based on feedback from consumers and clinicians. The streamlined content is now available in Arabic and Vietnamese. We are also exploring other accessibility options in the coming months.
The ACI Inflammatory Bowel Disease (IBD) Transition Working Group, led by Dr Astrid-Jane Williams, has finalised clinician and consumer surveys capturing the transition experience of young people with IBD. If you work in an IBD clinic, please complete and share the clinician and mapping survey with your colleagues and any recently transitioned adolescents who attend your service. The surveys are available here:
- Consumer experiences of IBD transition
- Clinician experiences of IBD transition
- Mapping of IBD services or clinics in NSW.
Welcome to our new co-chairs
It is with great pleasure that we welcome Dr Jane Ho and Lif O’Connor, who are taking on the roles of network co-chairs from Associate Professor Susan Towns and Mae Rafraf.
Susan and Mae have served the network for numerous years and their leadership will be a hard act to follow. We thank them wholeheartedly and encourage you to learn more about their insights into leading the network in this issue of Clinician Connect.
Dr Ho is a paediatrician who works as a staff specialist at The Sydney Children’s Hospitals Network. Dr Ho believes young people are full of promise and that support and interventions enhance their independence, self-management and transition to adult health services.
Lif O’Connor is a registered general, mental health and intellectual disability nurse, with extensive experience working in diverse settings. In her current role for the South Eastern Sydney Local Health District, Lif creates pathways for people with intellectual disability across their lifespan. She is also a Pokémon GO sensei, known across Sydney and parts of the US as 'the legend'.

Dr Jane Ho and Lif O’Connor.
Find out more and contact the Transition Care Network.
Keep up to date on the latest activities across our networks, and get involved in key projects that help drive improvements in healthcare.