Information guide for patients and carers
You have been referred for parenteral nutrition (PN). This fact sheet will help you to understand what this is and how it may affect you.
What is parenteral nutrition and why is it needed?
When you eat, food passes from the stomach into the digestive tract (also known as the bowel or gut), where it is broken down and absorbed into the body. However, you may not be able to digest food in the normal way. There might be various reasons for this and you can discuss this with your medical team.
When your digestive tract is not working, you still need nutrition. This is when you need PN (sometimes called total parenteral nutrition or TPN).
PN is a sterile solution containing nutrients normally found in food – protein, carbohydrate, fat, water, vitamins, minerals and electrolytes. The solution is infused straight into the bloodstream, bypassing the digestive tract.
You will need PN until your digestive tract is working properly (absorbing nutrients). Just like eating and drinking after any illness, improving your nutritional state takes time. This may include slow weight gain, if required.
How does it work?
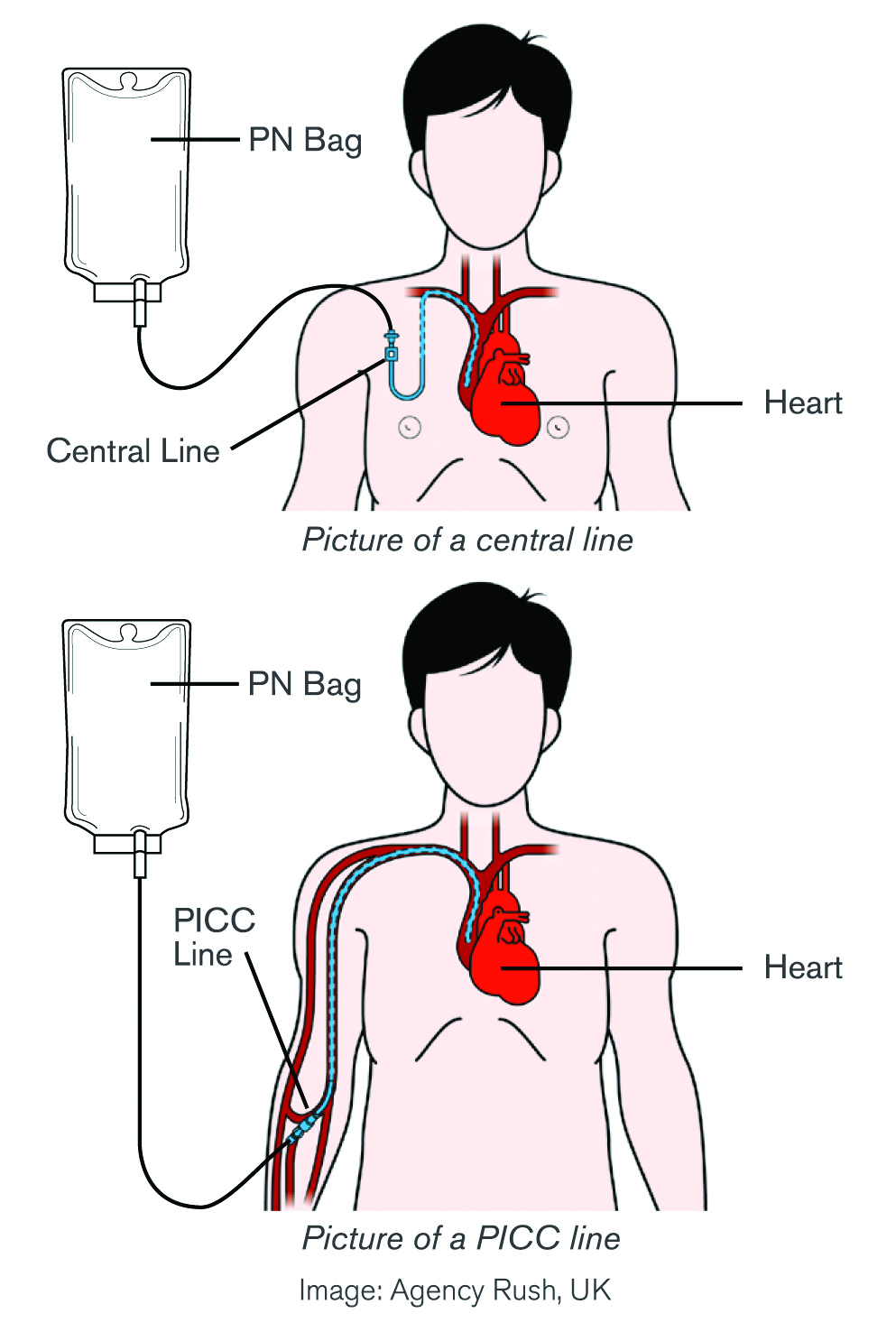
PN is given via a drip (intravenous infusion) into the bloodstream using an infusion pump. PN is a concentrated solution so it must be given into a large (central) vein. Medical and nursing staff will often use the terms ‘line’, ‘catheter’, ‘device’ or ‘port’.
Your medical team will discuss the most suitable type of device or catheter and way of accessing this large vein when obtaining your consent.
The pictures show two examples of how PN can be given via a central line. It could be called a PICC line (a peripherally inserted central catheter).
PN is usually infused continuously over 24 hours. The PN bag is changed about the same time each day.
What will happen while on PN?
During your PN therapy you will be monitored closely. This will include regular blood tests, temperature, pulse and weight checks. Nursing staff will care for your catheter on a regular basis. It is very important to keep the catheter clean.
This helps to reduce the risk of infection. Hand hygiene must be maintained at all times.
Tell the nursing staff and medical team immediately about any of the following:
- painful or uncomfortable catheter site
- a leaking catheter
- fever, shakes, shivers or sweats.
Will I feel hungry or thirsty?
On PN, you may not feel hungry or thirsty at all. This is because you are receiving all of the nutrition you need. If you are feeling hungry or thirsty, talk to your medical team.
Can I eat and drink?
This depends on your medical condition. This will be explained by your medical team.
Oral hygiene and mouth care
Good mouth care is important even when you’re not eating or drinking. Cleaning your teeth and/or having regular mouth washes will help with oral hygiene. If your mouth is dry, tell your medical team.
Will I still need to go to the toilet?
Yes. Your bladder should work normally. The bowel still produces secretions if you are not eating.
What happens if my dressing is loose or coming off?
The catheter site must remain clean and dry. If the dressing is wet, loose or soiled, tell your nurse immediately.
Can I shower?
Yes. Your catheter site and dressing must be kept dry in the shower. Baths are recommended for children. If your catheter site or dressing becomes wet, tell your nurse immediately.
Benefits and risks
The medical team will discuss the benefits and potential risks of PN with you.
Catheter (intravenous)
A tube that can be inserted into a vein to give medications or fluids straight into the bloodstream.
Digestive or gastrointestinal tract (sometimes called gut)
All the organs that break down food and absorb the nutrients that are used by the body for fuel. The organs of the digestive tract are the mouth, oesophagus, stomach, small and large bowel (intestine), rectum and anus.
Intravenous infusion
A method of giving drugs and/or fluids continuously, through a needle or catheter inserted into a vein.
Acknowledgements
This information sheet was developed by the Gastroenterology and Nutrition Networks, Parenteral Nutrition Down Under and IBD Support Australia Inc.