Five key solutions, targeting referral, bookings management and care delivery were co-designed with consumers with the aim of improving access and increasing the number of women commencing specialised antenatal care earlier in pregnancy. Outcomes achieved include an increase in clinic capacity with 524 appointments freed up for other patients (in eight months), a reduction in waste and a more streamlined antenatal service aligned to recommended practice guidelines.
Aim
Reduce risk and improve access for women referred to the Auburn Hospital antenatal clinics (ANC) through a high-quality, woman-centred service.
- 50% of women referred commencing antenatal care before 14 weeks gestation by December 2020 in line with contemporary best practice.
- 50% of patients no longer requiring antenatal care have care transferred more than 24 hours before the next scheduled appointment by December 2020, allowing appointments to be used for other patients.
- The percentage of referrals entered into the patient administration system is increased to 100% by December 2020.
For patients
- Improved health outcomes for mothers and babies through early detection and intervention and comprehensive care planning and access to education and psychosocial support.
- A positive pregnancy experience and transition to motherhood.
- Reduced wait times.
For staff
- Streamlined processes to enable more efficient workflows, better coordination of services, communication and utilisation of clinical resources (reduced waste).
- Improved role delineation, accountability and job satisfaction.
- Patients are encouraged to take responsibility for their health.
For the organisation
- Strengthened partnerships with general practitioners (GPs).
- Improved key performance indicators in performance and reporting.
- Increased revenue through improved capacity and data quality to maximise activity capture.
- Reduced costs associated with unnecessary birth unit and emergency department presentations.
Background
The Auburn Hospital ANC provide antenatal services to pregnant women within the Cumberland Local Government Area. On average, there are 1500 births per annum. However only 4% of these women are commencing antenatal care by 14 weeks gestation, in line with contemporary best practice. This means 24 out of 25 mothers and babies are at an increased risk of a compromised healthy outcome. Key gestational milestones and diagnostic screening are missed and access to comprehensive care planning, intervention, information and psychosocial support is delayed. One in two women are referred late.
Serving one of the fastest growing and most culturally and linguistically diverse regions in NSW, with total fertility rates well above both state and national levels, the local area hosts pockets of significant socioeconomic disadvantage.1-2 One in five women seen have gestational diabetes and two in five have a high body mass index, placing them at further risk during pregnancy.
Existing systems and processes, including bookings, referral management and communication with internal and external stakeholders, are not meeting the growing demand for outpatient antenatal services provided by Auburn Hospital. Women consistently reported feeling anxious and worried whilst waiting for an appointment.
Implementation
Using the redesign methodology and engaging with key stakeholders, three key issues were identified. These were addressed through implementation of five solutions.
Issue 1: Poor communication with internal and external stakeholders
- Lack of communication between birth unit and ANC when a patient gives birth resulting in lost clinic capacity and retrospective cancellation of appointments when antenatal care is no longer required.
- 60% of referrals received were incomplete or missing essential information required for accurate and timely triage.
- Two in three GPs reported communication issues (no communication with GPs from referral to birth).
Issue 2: Inefficient documents management processes
- Only 4% of referrals were accurately registered in the patient administration system (iPM) leading to an inability to effectively track referrals and potentially lost revenue.
Solution 1: Transfer of care when antenatal care is no longer required
- Daily birth register checks by the birth unit administrative staff and proactive cancellation of antenatal appointments when antenatal care is no longer required.
Quick win: GP hotline
- Establishment of a hotline, during business hours, allowing GPs direct access to a specialised antenatal registered midwife for patient enquiries.
Solution 2: Referral management and information
- Development of a referral management flowchart including a robust referral screening and acceptance procedure (incomplete referrals no longer accepted).
- Enhancement of existing notification letters to patients and GPs with the addition of written notification to GPs when a referral is received.
- Staff re-training to promote accurate and consistent referral registration into iPM
Issue 3: Outdated booking management procedures
- No clearly defined triage or attendance management processes.
- Lack of incorporation of the Australian College of Midwives’ National Guidelines for Consultation and Referral into care provision resulting in all patients (including low-risk) being unnecessarily seen by a doctor.3
- Booking schedules were outdated and not set-up to meet varied patient complexity (lost capacity). Peer services were found to be seeing five patients for their first visit ‘booking in’ consultation, per midwife per day, whereas Auburn Hospital ANC were only seeing four.
Solution 3: Triaging guidelines
- Phase 1: Establishment of clinical priority category triage procedure with recommended time frames for women to be seen according to clinical need. (Figure 1)
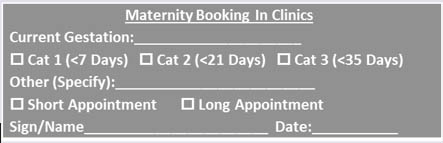 Figure 1: Clinical priority category triage stamp developed, Maternity Booking In Clinics, Auburn Hospital
Figure 1: Clinical priority category triage stamp developed, Maternity Booking In Clinics, Auburn Hospital - Phase 2: Incorporation of the Australian College of Midwives’ Guidelines into ANC provision and identification of Category A ‘low-risk’ patients.
- Phase 3: Category A medical file review to assess appropriateness for patient to remain under Midwifery-Led Model of Care (doctor’s appointment not required).
Solution 4: Attendance management procedure
- The existing Western Sydney Local Health District procedure for managing outpatient attendance was adapted to suit the needs of pregnant women whilst remaining aligned to the NSW Health Outpatient Services Framework.
4
Solution 5: Booking schedule restructure
- The maternity booking in clinic schedule was restructured to include short (75 mins) and long (105 mins) appointment slots (all appointments previously 105 mins). The new schedule meant consultation time, allocated at time of triage, was appropriate for each woman and an additional woman could be booked in per midwife per day; thus improving clinic capacity and providing faster access to antenatal care.
Four out of five solutions have been piloted and successfully implemented. Due to COVID- 19, implementation of Solution 5 has remained on hold since March 2020.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
August 2019 – December 2020
Implementation sites
Auburn Hospital, Western Sydney Local Health District (WSLHD), potential roll-out to other WSLHD facilities planned.
Partnerships
Agency for Clinical Innovation- Centre for Healthcare Redesign, WSLHD Community & Consumer Partnerships Team, WentWest (Primary Health Network).
Results
Objective 1
Despite COVID-19 restricting implementation of the new booking schedule (solution 5), an increase from 4% to 17% in the <14 weeks cohort was seen post implementation of solution 3, phase 1 (clinical priority category procedure).
Although a continued effort towards the 50% target exists, an overall shift in women commencing care much earlier in pregnancy was apparent (Figure 2). Women commencing care later in pregnancy, i.e. >18 weeks, gestation continues to decline.
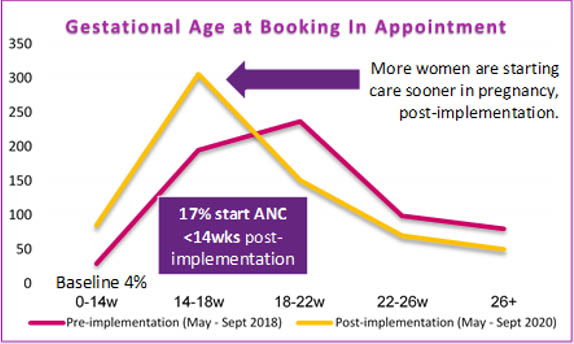
Figure 2: Gestational Age at Booking In Appointment, Auburn Hospital ANC (May- Sept 2018/2020)
Objective 2
The success of objective 2 was measured by monitoring the percentage of total ANC appointments cancelled more than 24 hours before the next scheduled appointment for women no longer requiring antenatal care i.e. after giving birth. By September 2020, a 50% increase from 19% to 69% was seen post implementation of solution 1 (transfer of care) in January 2020 and solution 2 (attendance management procedure) in March 2020. These results were consistently maintained above the 50% target (Figure 3).
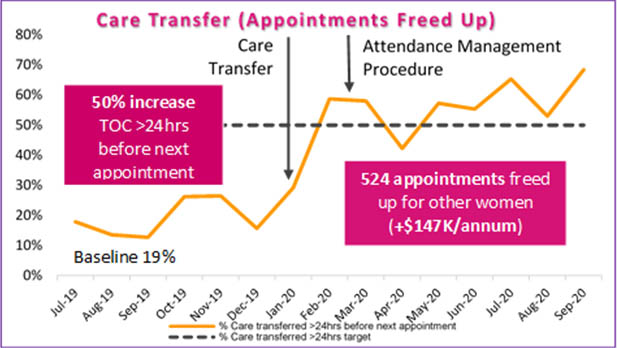 Figure 3: Care transferred >24 hours before the next appointment, Auburn Hospital ANC (Jul 19- Sept 20)
Figure 3: Care transferred >24 hours before the next appointment, Auburn Hospital ANC (Jul 19- Sept 20)
In eight months, a total of 524 appointment slots were freed up for other patients. This was almost a 4% capacity increase across all ANC, generating additional hospital revenue estimated at over $147,000 per annum. Positive feedback and a reduction in time wasted screening clinic lists each day’ was reported by midwifery staff.
Objective 3
Refresher training for referral registration, close monitoring and feedback of performance to administrative staff resulted in referral entry rates into iPM dramatically increasing by 96% (Figure 4), with the project’s phase 1 target (50% by August 2020) achieved by December 2019 and the phase 2 target (100% by December 2020) achieved by September 2020.
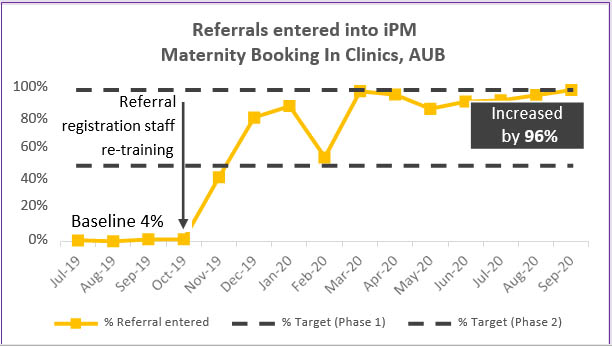 Figure 4: Referrals entered into iPM, Auburn Hospital Maternity Booking In Clinic (Jul 19- Sept 20)
Figure 4: Referrals entered into iPM, Auburn Hospital Maternity Booking In Clinic (Jul 19- Sept 20)
Other key outcomes and reported benefits
Referral information
Through implementation of a robust referral screening and acceptance procedure, the incomplete referral rate was reduced by 43%, from 60%, to 17% in five months, achieving the 25% target (Figure 5). Calls to general practices were also reduced by 43%.
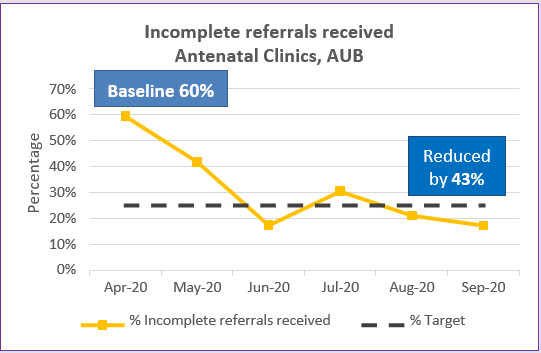
Figure 5: Incomplete referrals received, Auburn Hospital ANC (Apr- Sept 2020 )
Key performance indicators
An improvement in meeting the NSW Ministry of Health key performance indicators for triage of referrals within five days of receipt and scheduling an appointment within five days of triage was seen. During testing and three month spot check audits, the service consistently remained above 98% for both performance measures (baseline 60% and 27% respectively), reducing unnecessary delays.
“Improves communication with GP’s” (ANC Midwife)
“It makes a difference having the results sent with the referral” (ANC Midwife)
Model of care
Once 100% compliance was successfully maintained for correct assignment and documentation of an Australian College of Midwives’ Guideline category, daily medical file reviews for women identified as meeting the criteria for continued management under a Midwifery-Led Model of Care (Category A) were commenced. In 11 weeks, new patient demand for the antenatal doctors’ clinic was reduced by 43%, equating to an average of 13 patients less per week requiring medical review. In addition to reducing workloads and freeing up doctors to see more complex ANC patients, midwifery staff reported an ability to ‘take ownership and build rapport with patients sooner’.
Did not attends
Of the 524 appointments made available for other patients (Figure 3), 13% were attributed to patients being effectively discharged and the GP notified post implementation of the attendance management procedure. In seven months, did not attend rates were reduced from 10% to a sustained average of 7% in the midwifery-led clinics (target 8%). More clearly defined roles for midwifery and administrative staff, a reduction in task duplication and time spent attempting to contact patients after failing to attend their appointment were reported.
Patient experience
Using the assistance of health care interpreters, bilingual health care workers and consumers, patient experience was measured using the My Experience Matters survey platform, pre and post implementation. A marked improvement was seen in the patient’s perception of time spent waiting for an appointment with an increase from 57 to 81 weighted average score out of 100 seen post implementation (benchmark 85).
Revenue
Analysis of comparative financial figures from November 2018 to August 2019 and November 2019 to August 2020 post implementation of project solutions confirmed additional revenue of $72,623 generated for the service.
“The waiting time has improved a lot…" (Patient)
“The GP hotline is very helpful…timely access to advice” (Local GP)
Lessons learnt
- Strong sponsorship and reinforcement are key to project success.
- Plan early and manage time effectively.
- Stakeholder engagement and communication strategy are crucial when generating buy in and maintaining momentum.
- Carefully stage implementation to avoid change fatigue.
- Trust redesign methodology, don’t jump ahead.
- Partnering with consumers, use feedback to guide solution direction.
- Be willing to adapt to unexpected changes in the environment.
- Leverage influence of champions.
- Recognise and celebrate success.
References
- Australian Bureau of Statistics 2015, Australian Bureau of Statistics Belconnen, ACT, viewed 1 September 2019,
- WSLHD Social and Health Atlas, Epidemiology and Health Statistics. 2018, viewed 1 September 2019,
- Australian College of Midwives. National Midwifery Guidelines for Consultation and Referral, 3rd edition, Issue 2. NSW; 2014.
- NSW Government, Health. Outpatient Services Framework. NSW: NSW Government, Health; 2019.
Further reading
- Australian Government, Department of Health. Clinical Practice Guidelines, Pregnancy Care. Australia: Australian Government; 2019.
- NSW Health. NSW Health Strategic Priorities 2019-2020. NSW: NSW Health; 2020.
- NSW Ministry of Health. NSW Mothers and Babies 2017. NSW: NSW Ministry of Health; 2018.
- The Royal Australian and New Zealand College of Obstetrics and Gynaecologists. Antenatal Care during Pregnancy. 2016.
Contact
Julianne Harvey
Project Lead, Innovation & Redesign
Western Sydney Local Health District
Phone: 0437 232 189
Julianne.Harvey@health.nsw.gov.au
Helen Mou
Clinical Midwifery Consultant
Maternity Services, Auburn Hospital
Western Sydney Local Health District
Phone: 0447 302 513
Helen.Mou@health.nsw.gov.au
