The Paediatric Access Support Service (PASS) aims to transfer patients to and from Sydney Children’s Hospitals Network (SCHN) inpatient settings efficiently. This would reduce associated workload, and improve the patient and staff experience.
Our vision includes a Network-wide service that will coordinate patient transfers to and from SCHN to ensure the provision of best patient care with the right team, in the right place and at the right time.
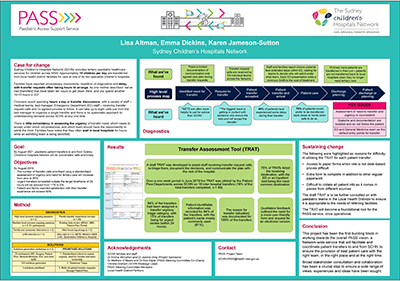
The first building block of the PASS project is the implementation of a process for all staff receiving transfer request calls that will help them triage, document the decisions and communicate the plan with the rest of the hospital.
View a poster from the Centre for Healthcare Redesign graduation, August 2019.
Aim
By August 2021, paediatric patient transfers to and from Sydney Children's Hospitals Network will be coordinated, safe and timely.
Benefits
- Improved experience for patients and families navigating the health system.
- Improved communication and processes between SCHN and local health facilities and general practices.
- Cost savings to the health system through emergency department (ED) avoidance strategies including direct ward-to-ward transfers and facilitating care in the lowest cost settings.
- Reduced travel burden for regional and remote families, managing care closer to home.
- Reduced administrative burden for clinical staff.
Background
The SCHN provides tertiary paediatric healthcare services for children across NSW. Approximately 15 children per day are transferred from local health district facilities for care at one of its two tertiary children’s hospitals. Families have reported unnecessary movements, repetition of diagnostics and delay, with transfer requests often taking hours to arrange. As one mother described: “The biggest issue is getting in contact with someone who knows the kids and will accept the transfer and we’ve had [transfers] that have taken ten hours to get down there, and you spend another 10-15 hours in ED”.
It can take up to eight calls just from the bed manager to organise a single transfer, with 54 different access points to our services. Medical teams, the bed manager, patient flow team and ED staff all receive transfer request calls with no agreed process to follow, and clinicians report spending hours a day in transfer discussions.
There is no systematic approach to understanding demand across the Network at any one time and little consistency in assessing the urgency of transfer need. A need to better coordinate transfers and identify which team should have responsibility to admit the child has been identified, with 67% of transfers arriving after hours to our emergency departments.
Families have noted that they often wait in local hospitals for hours while an admitting team is being identified, with 48% of families transferred to SCHN facilities reporting that they experienced some delay during their transfer. Around 75% of our families have identified that they would prefer to be transferred back closer to home when safe to do so.
Implementation
Solutions generation workshop (November and December 2018)
Two solutions generation workshops were held across SCHN with broad representation from ED, surgery, patient flow, general medicine, the intensive care unit and ward staff. A total of 125 solutions were generated, with the following three prioritised by the PASS Steering Committee.
- Refer all patient transfer requests through patient flow.
- Telephone triage: Triage of transfer requests into four categories – emergent, urgent, non-urgent and ‘stay with support’.
- Standardise the criteria required to assess urgency, the need for transfer and team ownership.
Solutions co-design (February 2019)
A draft Transfer Assessment Tool (TRAT) was developed and tested at two co-design workshops, using role-play. Feedback was received surrounding:
- the length of the form
- the method of ‘Identify, Situation, Background, Assessment and Recommendation’ (ISBAR), which was identified as the preferred documentation method
- expectation upon whose role it would be to complete it.
Pilot phase (17 – 23 June 2019)
Over a one-week period, the patient flow departments across SCHN piloted the TRAT on 16 inter-hospital transfers, 18% of the total transfers completed (n = 89). Guidelines, flow charts and feedback forms were also developed to assist with the pilot. Feedback obtained from the trial has been used to make changes to the tool.
Further consultation
The TRAT is to be further consulted on with paediatric teams in the local health districts.
Implementation
The TRAT will become a foundational tool for the PASS service, once operational.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
August 2018 – October 2019
Implementation sites
- Sydney Children’s Hospitals Network
- The Children’s Hospital at Westmead
- Sydney Children’s Hospital, Randwick
Partnerships
- Centre for Healthcare Redesign
- Children’s Healthcare Networks
- Consultation with local health district partners
Results
Over a one-week period in June 2019 the TRAT was trialled by the patient flow department on 16 inter-hospital transfers across Sydney Children’s Hospitals Network.
- Around 94% (n = 15) of the transfers had been assigned a transfer urgency triage category.
- Around 75% (n = 12) of transfers were for urgent (<24 hours) review.
- Patient identifiable information was recorded for 94% (n = 15) of the transfers, with the patient’s name the mostly commonly used (81%, n = 13).
- Around 13% (n= 2) of the TRATs included both the patient’s name and their medical record number.
- The reason for transfer (situation) was documented for 100% (n=16) of the transfers.
- Around 75% (n = 12) of TRATs listed the receiving destination, with the ED or an inpatient bed being the most common destinations.
- Qualitative feedback received during the trial was based on the need for a more user-friendly form and requests for an electronic version.
Lessons learnt
- Consult broadly with stakeholders to ensure a wide range of views, experiences and ideas are sought.
- Be flexible in your consultation approach, and ensure multiple forums are held with mixed stakeholder groups.
- Take advantage of opportunities for informal or coffee meetings, or hallway chats.
- Maintain focus on your objectives and be aware of scope creep.
Further reading
- J Rosenthal, P Romano, J Kokroko, W Gu, M Okumura. ‘Receiving providers’ perceptions on information transmission during interfacility transfers to general pediatric floors, leading to delays in treatment and potentially impacting patient outcomes’, Hospital Pediatrics, vol. 7, no. 6, 2017, pp. 335 - 343
Contacts
- Karen Jameson-Sutton, After-hours Nurse Manager, Sydney Children’s Hospitals Network
- Lisa Altman, Clinical Services Alignment Lead, Randwick Precinct Redevelopment
- Emma Dickins, Integrated Care Lead, Sydney Children’s Hospitals Network