NSWHP flow cytometry model of service
Summary
NSWHP flow cytometry services have developed over time, with no coordinated strategic plan to provide optimal care to all patients and service to all doctors throughout NSW. The opportunity of this project is to investigate all possible models of service and determine the best way in which to deliver a world class, value based public flow cytometry service that is renowned for both excellence and innovation.
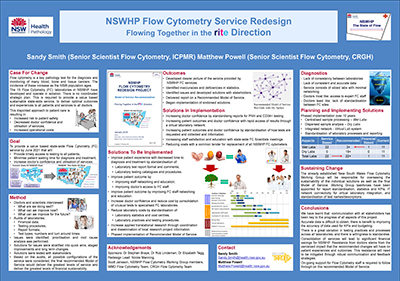
View a poster from the Centre for Healthcare Redesign graduation, May 2019.
Aim
Goal
To provide a value based statewide flow cytometry service that will:
- provide timely access to testing to patients, from metropolitan, rural and remote NSW
- minimise patient waiting time for diagnostic information and treatment
- increase doctors’ confidence and utilisation of out-patient services.
Objectives
- To increase the number of samples that are reported within turn-around-time (TAT) limits to above 95% (more than 43,000 tests) by financial year 2020/21.
- To increase the outpatient requests from discharged oncology in-patients from 90% in financial year 2016/17 to 100% in financial year 2020/21.
- To reduce per capita spending for flow cytometry testing in NSWHP laboratories by 10% by the end of financial year 2020/21.
Benefits
- Strategically planed, sustainable, statewide model of service.
- Increased patient safety through the delivery of high quality and timely results.
- Increased doctor confidence and utilisation of the service through a patient focused service.
- Increased demand for a high-performance service.
- Decreased incidence of patient sample recollection and retesting due to the integration and access to expert scientific staff.
- Increased patient care through support of all bone marrow transplant units throughout NSW.
- Increased opportunities for staff to thrive and innovate with collaboration and coordination.
- Increased opportunity for staff training and education through an integrated network of laboratories.
- Increased professionalism of service through consistent testing methodology and standardised reporting formats.
- Increased number of samples resulted and reported within clinically appropriate turn-around-time limits.
- Increased doctor confidence through positive encounters with expert flow cytometry scientific staff.
- Increased presence at doctor meetings for patient management such as multi-disciplinary team meetings.
- Decreased operational costs and wastage through common efficient processes.
- Increased service footprint without the proliferation of expensive instrumentation.
- Increased ability for succession planning throughout all levels of scientific staff.
- Increased buying power with vendors through a unified service.
- Increased opportunities for effective translational research through a strategically planned research service.
- Increased flexibility of configuration, adaptability to technological innovation and future proofing of the service.
Background
Flow cytometry is a key pathology test for the diagnosis and monitoring of many blood, bone and tissue cancers. Though these diseases are most commonly seen in young children and from middle age, they can affect people of any age.
NSW is seeing significant growth in these key age groups, the result of which is a forecast doubling of disease incidence and associated burden on NSWHP flow cytometry services over the next 10 years.
NSWHP flow cytometry service currently consists of 15 laboratories working in isolation, with no strategic structure to provide a value based sustainable state-wide service. These sites were set up independent of each other with different work practices and no formal channels for communication and collaboration. This disjointed approach to patient care results in:
- increased risk to patient safety through delayed and inconsistent results
- decreased doctor confidence and utilisation of the service due to inconsistent practices
- increased operational costs through inefficiencies and wastage.
Without a standardised strategic plan and appropriate model of service, the current service is unlikely to cope with the forecast increase in demand for a high quality, sustainable public service.
Implementation
- Doctors and scientists were interviewed and surveyed to assess what our current service is doing well and areas in which it could be improved now and in the future.
- Audits of laboratories, test numbers and financial data were undertaken to compile an accurate picture of the service as we currently provide it.
- Solutions were identified for current issues that could be implemented independent of the final model of service delivered.
- Networking of current flow cytometry laboratories began in July 2018 with the first scientific staff forum.
- Standardisation of flow cytometry result reporting began in October 2018.
- Preparation for a state wide it solution for flow cytometry services began in October 2018.
- Based on the audits, all possible configurations of the service were considered, and then models of service were developed that could deliver the greatest levels of service and deliver the greatest levels of financial sustainability.
- A model of service was then developed that incorporates the greatest strength of each model.
- The recommended model of service incorporates a reduced number of flow cytometry laboratories in which samples are processed which will deliver financial savings, supported by a network of virtual flow cytometry laboratories that will enable continued and expanded levels of interaction with and service to doctors.
- The recommended model of service depends upon eight key requirements to be in place before implementation, with staffing, diversified clinical interaction, virtual laboratory network, process harmonisation, CD34 testing, sample transport, research collaboration and space.
- These requirements are scheduled to be implemented over the next three to five years, and must be in place before implementation of the model of service can start.
- Complete implementation of the new model of service is planned to occur over a 10-year period.
- The report on the recommended model of service was delivered to project sponsors in January 2019.
Status
Future initiative - These include those that are in the operational plan and/or an active work project.
Dates
- Project Initiation: April 2018
- First standardised report format developed and delivered for peer review: January 2019
- Implement regular educational meetings for scientific staff: January 2019
- Model of service recommendation report delivered: February 2019
- Approval of model of service recommendations for implementation by project sponsors: March 2019
- Develop and implement performance index for all laboratories: April 2019
- Implementation of state wide data server for centralised storage of patient data files: June 2019
- Begin process for purchase of new state of the art instrumentation: June 2019
- Begin process for purchase of virtual laboratory system: June 2019
- Install new instrumentation and virtual laboratory system: June 2020
- Project completion: June 2021
Evaluation
Results of this project will be evaluated throughout the implementation process. Several measures and metrics will be employed to do this:
- increase in test numbers above normal forecast growth
- increased proportion of tests performed and reported to doctors within clinically approved time frames
- reduction in per capita cost of testing for all flow cytometry assays
- reduction in recollection of patient samples for testing due to laboratory error
- increased proportion of laboratories using the standardised result report format for all flow cytometry tests
- increased proportion of laboratories using the standardised testing procedures for all flow cytometry test performed
- increased numbers of clinical haematology units with direct access to expert flow cytometry scientific staff
- new state of the art cytometers purchased for laboratories
- surveys and forums to assess levels of doctor satisfaction
- surveys and forums to assess levels of scientist satisfaction.
Lessons Learnt
- Communication with all stakeholders is key.
- Communication with technology is good, face to face is better.
- Ask questions: while the person you are talking to might not know the answer, they might know who does.
- It takes less time to find the right person for the job than it does to try to do everything yourself.
- Always monitor your sponsors’ expectations and be sure to meet them.
- Accurate data is not always possible to obtain.
- Accurate statistics are a rare thing.
- Work practices can vary greatly across individual sites despite being part of the same organisation. Don’t assume everyone does things the same way as you do. Don’t assume anything!
Contacts
Sandy Smith
Senior Scientist Flow Cytometry
Institute for Clinical Pathology and Medical Research
Westmead Hospital
Phone: 02 8890 6275
Sandy.Smith@health.nsw.gov.au
Matthew Powell
Senior Scientist Flow Cytometry
Diagnostic Pathology Unit
Concord Repatriation General Hospital
Phone: 02 9767 5886
Matthew.Powell@health.nsw.gov.au