A project which aims to improve access to care for mental health patients by reducing their length of stay in the emergency department (ED) and reducing barriers to discharge from the Caritas, the mental health unit (MHU) in St. Vincent’s Hospital.
Aim
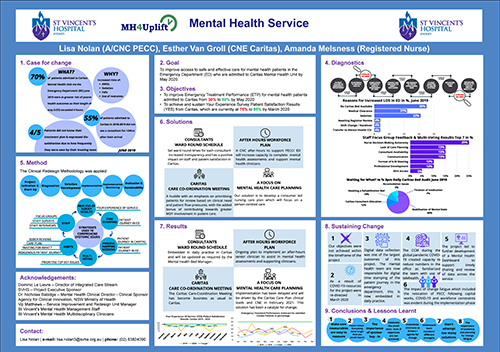
To improve access to safe and effective care for mental health patients in the Emergency Department who are admitted to Caritas (MHU) by increasing Emergency Treatment Performance (ETP) for mental health patients admitted to Caritas from 25% to 50% by May 2020, and achieve improvement of patient satisfaction ‘Your Experience of Service’ (YES) survey results in Caritas MHU from 75% to 85% by March 2020.
Benefits
- Better patient experience of care for mental health consumers.
- Reduction in adverse outcomes for mental health consumers.
- Improved patient safety.
- Improved staff satisfaction and stronger staff morale.
- An upskilled and empowered mental health nurse workforce.
- Increased cohesion and communication within the multidisciplinary team.
- Improved communication and collaboration between the multidisciplinary team, mental health consumers, their families and carers.
- Mental health consumers with an improved understanding of their care and treatment planning..
Program status
Program dates
The project was initiated in April 2019.
Some of the major milestones for the project were:
- After-hours Emergency Department workforce pilot – July 2019
- EDIS Electronic Data Collection Go Live – October 2019
- Caritas consultant roster Go Live – May 2019
- Caritas Care Coordination Meeting pilot – October 2019. Go Live - November 2019
- Care planning in Caritas – Working party assembled January 2020, implementation postponed due to COVID-19. Implementation TBC.
Evaluation phase TBC due to staffing crisis and COVID-19 restrictions.
Status
Implementation - The project is ready for implementation or is currently being implemented, piloted or tested.
Background
70% of the 49 mental health patients admitted to Caritas MHU via the ED in June 2019 were put at greater risk of poor health outcomes when their length of stay in ED exceeded four hours. Mental health consumers exposed to long periods in the ED are at an increased risk of leaving the hospital against medical advice, being given more sedating medications thus experiencing a fall or being physically restrained when their stay in the ED is greater than four hours.
- Improving patient flow will improve the mental health consumer’s experience of care, as well as staff satisfaction.
- 55% of patients admitted to Caritas (mid July 2018-2019) did not see a psychiatric consultant for 24 hours or more after their arrival at Caritas (MHU).
Four out of five consumers reported dissatisfaction with the frequency of time spent in communication with members of their multi-disciplinary team.
Caritas was performing 20%+ below target in the Your Experience of Service (YES) patent satisfaction survey results, achieving just 61% in June and 64% in July results.
An audit of nursing care plans was carried out in Caritas in July 2019. There were 25 mental health consumers admitted at the time of the audit.
- 14 out of 25 consumers had a nursing care plan which had been completed by a nurse.
- Zero out of 25 care plans had evidence of patient involvement or goals which were individualised.
- Four out of 25 care plans had a date set for the goal target.
- Eight out of 25 had use of jargon which may not have been easily interpreted by the consumer.
- Two out of 25 care plans had a set date for review or had been updated in some way since initial completion.
- One out of 25 was signed by a primary carer.
- One out of 25 had evidence of a multidisciplinary team approach to care.
- Zero out of 25 had goals with a recovery focus.
The audit highlighted that the current NSW health nursing care plan is not utilised effectively by our mental health nurses in Caritas. It is therefore unsurprising that four out of five consumers stated that they had minimal understanding of their treatment plan or their estimated date of discharge from hospital.
Implementation
Initiation
We defined and developed a clear understanding of what the project is, the scope of it and how we planned to tackle the variables such as stakeholders, risks and issues within the organisation. We established sponsorship and steering committee governance to ensure project ownership and organisational support.
Diagnostics
Involved discussions with key stakeholders to understand the ‘as is’ of what is happening today within the mental health service at St. Vincent’s. This allowed us to establish a baseline in order to identify what needs to change. Diagnostic tools included root cause analysis, focus groups, staff surveys and staff interviews, time stamping of the patient journey, file audits, process mapping, patient feedback and surveying of staff and patients. This data highlighted the systemic issues within the service, allowing the team to focus on triple aim solutions.
Solutions
We developed solutions in conjunction with our key stakeholders, with a focus on patient and staff satisfaction. A total of 10 solutions were reduced to four key solutions with the use of multi-voting by the Steering Committee. Our four key solutions were as follows.
- To establish a regular schedule of ward round times for all psychiatric consultants in Caritas.
- Develop an after-hours mental health workforce plan to support patient flow priorities across the mental health service.
- Develop a 15-minute 'Care Co-ordination Meeting' in Caritas replacing current 30+ minute morning meeting.
- To develop a recovery focused care plan and methods for incorporating use of the care plan into daily practises.
These solutions were supported by executive sponsor and steering committee.
Implementation
During the trial of rostering senior staff in the after-hours space we discovered a key issue in data collection. The data was collected manually by the mental health team in the Emergency Department. By introducing electronic data collection using the Emergency Department Information System (EDIS) we developed the mental health service capacity to record the patient journey electronically. This has been one of the most beneficial outcomes of the project.
The after-hours workforce plan has not yet been implemented, as the trial failed to give clear quantitative data in relation to how we can predict times of high acuity within mental health. This was a direct result of the issues in data collection at the time of the trial and the proven lack of predictability within the mental health sector. The project team has focused on accurate and timely data collection, which can facilitate improved processes to increase communication and streamline data within mental health. The solution itself is being explored by the senior management team who are working to create provisions for a CNC role for after-hours and on weekends. A project team member has developed a mental health dashboard which displays details of the patient journey electronically as a result of this initial finding.
Care planning and improved collaboration between the multidisciplinary team and consumers in developing treatment goals is an ongoing issue in Caritas (MHU). The solution has been trialled but not yet successfully implemented, as a result of disruptions during the global pandemic of COVID-19 and change fatigue amongst staff. Compliance with care planning remains poor in Caritas. Solution owners continue to develop implementation planning in the future.
Evaluation and sustainability
It became clear early on that manual data collection would be the biggest barrier to the success. While there was strong stakeholder involvement, through ownership of solutions and change agents early in the project, the collection of manual data was not foreseen as the level of risk it held. One of the drivers of the project was to work closely with emergency and administrative staff to adapt the current electronic systems by applying electronic data flags on the patient's journey through the ED. The Care Coordination Meeting has become ingrained in culture and daily morning schedule in Caritas. It has increased communication between the multidisciplinary team, reduced time wastage, as well as improved patient care.
Staffing shortfalls and the evolution of the global pandemic COVID-19 led to organisational stress which became a barrier for implementation and sustainability. Resource requirements and restructuring led to a change in focus, during a key period of implementation, which meant that the solutions lost momentum. These elements resulted in change fatigue within the service, impacting on agent capacity and competency. This in turn impacted motivation for change within the overall mental health team.
Implementation sites
St Vincent’s Hospital, Mental Health Department
Results
- The aim of the project has not yet been achieved.
- Final evaluation of the project TBC.
- Discharge before 11am statistics: 5% improvement in DC before 11am statistics.
- Emergency Treatment Performance has not improved.
- Your Experience of Survey (YES) results have not improved. Feedback from patients highlight dissatisfaction due to leave restrictions and staffing shortfalls that impacted nurse to patient ratios, however this can be attributed to multiple reasons.
Lessons learnt
- Implementation was challenging.
- Be careful to ensure that all process measures are sustainable.
- Try to utilise established systems to measure solutions, rather than developing new systems.
- Try to have measurables that are not multi factorial as it is difficult to identify specific impacts due to multiple, potentially attributing, causes.
- Be mindful of the scale of solutions, i.e. the care planning solution is so large scale that it could have informed a redesign project by itself.
Further Reading
- Australian Commission on Safety and Quality in Health Care. National Safety and Quality Health Service Standards. 2nd ed. Sydney: NSW Australian Commission on Safety and Quality in Health Care; 2017.
- Bowers L, Crowder M. Nursing staff numbers and their relationship to conflict and containment rates on psychiatric wards—A cross sectional time series Poisson regression study. International Journal of Nursing Studies. 2012;49:15-20.
- Cunningham PA. The future of community-centred health services in Australia - an alternative view. Australian Health Review. 2012;36:(2):7.
- NSW Government Ministry of Health. KPI and Improvement Measure Data Supplement. Mental Health Consumer Experience: Mental Health consumers with a score of Very Good or Excellent (%). Sydney: NSW Ministry of Health; 2018.p.131
- NSW Mental Health Commission. Living Well: A Strategic Plan for Mental Health in NSW. Sydney: NSW Mental Health Commission; 2014.
- System Information and Analytics Branch. NSW Health 2018, InforMH. Sydney: NSW Ministry of Health; 2018.
- Pearlmutter MD, Dwyer KH, Burke LG, et al. The practice of emergency medicine/original research: Analysis of Emergency Department Length of Stay for Mental Health Patients at Ten Massachusetts Emergency Departments. Annals of Emergency Medicine. 2017;70:193-202.
- Short AE, Short KT, Holdgate A.et al. Research Paper: Noise levels in an Australian emergency department. Australasian Emergency Nursing Journal. 2011;14:26-31.
- Totman J, Hundt GL, Wearn E, et al. Factors affecting staff morale on inpatient mental health wards in England: a qualitative investigation. BMC Psychiatry. 2011;11(1):68-77.
Contacts
Lisa Nolan A/Clinical Nurse Consultant
Psychiatric Emergency Care Centre
St. Vincent’s Hospital
Phone: (02) 8383 4090
lisa.nolan@health.nsw.gov.au