The St George Acute Mental Health Unit (MHU) developed a new model of care that increased the involvement of clients in their clinical care and discharge planning, through improved communication between mental health clients, clinicians and nursing staff.
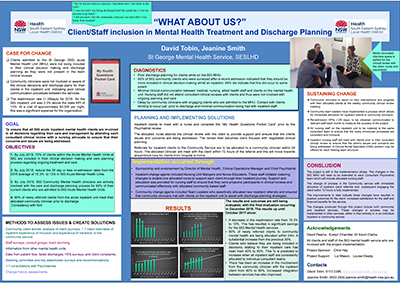
View a poster from the Centre for Healthcare Redesign graduation, December 2017.
Aim
To increase the number of clients who are admitted to the St George Acute MHU and included in their clinical care reviews and discharge planning, to 70 per cent by October 2018.
Benefits
- Improves discharge planning, goal setting and outcomes for mental health clients.
- Enhances communication between mental health clients, clinicians and nurses.
- Increases referrals and access to community clinicians for MHU clients.
- Increases involvement of the client in their treatment and discharge planning.
- Improves client and staff satisfaction with the St George Acute MHU service.
- Reduces unplanned readmissions to the MHU within 28 days of discharge.
- Delivers care in line with the SESLHD Mental Health Clinical Services Plan.
Background
Prior to the project, the St George Acute MHU experienced poor clinical communication between medical staff, clinical staff and clients. There was limited evidence of clients being included in their treatment and discharge planning, with clients providing feedback such as: ‘I was not informed about the medication I was made to take’ (YES Survey, December 2016) and ‘Sometimes when I summoned the courage to ask questions about my care, they were minimised or ignored’ (Compliments and Concerns Group, February 2017). There was also a lack of structure for communication between Community Mental Health Service staff and St George Acute MHU staff. Clinicians at St George Acute MHU were sometimes unaware that important treatment or discharge planning meetings were taking place and as such were not part of the clinical decision-making process.
There is a relationship between the level of client involvement in their treatment planning and their ability to follow the instructions in their discharge plan. Not understanding or following a discharge plan can lead to clients being readmitted to hospital shortly after discharge. In 2016, the readmission rate within 28 days of discharge at St George Acute MHU was 15.3 per cent, higher than the statewide target of 13 per cent. In addition to the negative impact on healthcare outcomes of clients, unnecessary readmissions are a significant cost to the organisation, at approximately $3000 per night for an acute MHU bed. Reducing readmissions down to 12 per cent by July 2018 is expected to result in an average saving of $34,000 per month.
By improving clinical communication and engaging clients in their treatment and discharge planning, it was anticipated that St George Acute MHU would be able to reduce readmission rates and improve the healthcare journey of its clients.
Implementation
- A detailed analysis of the MHU was undertaken, to identify gaps in the service and why these had occurred. Two root causes were identified:
- there was no formal opportunity for inpatients to discuss their treatment and discharge plan with the staff responsible for implementing those plans
- the structure of the nurse roster and delays in allocating a community clinician for referred clients prevented staff from consistently engaging with clients while in the MHU.
- Surveys, consultation forums, one-on-one interviews and detailed client journeys were completed with a diverse range of staff and clients. These included inpatient clients, discharged clients, clinicians, nurses, medical staff, peer support workers and other key stakeholders.
- A new model of care was designed and implemented, as follows:
- a consultant psychiatrist was engaged for set appointment times to review MHU clients, replacing the previous process of unplanned reviews
- two nursing staff were allocated responsibility for the consultant’s clients, including preparation of the client for their clinical review (using the My Health Questions Pocket Card) and attendance at their review
- nursing staff communicated the treatment plan to colleagues, to ensure it was implemented in conjunction with the client
- a community clinician attended the clinical review when required and was actively involved in treatment and discharge planning with clients
- community teams allocated new clients within 24 hours of referral, providing an in-reach service within 72 hours of admission.
- Education was provided to nursing staff on increasing engagement with clients and how to advocate on their behalf in clinical reviews.
- The initial pilot using one consultant psychiatrist, two nursing staff and seven clients will be expanded to all consultant psychiatrists, nurses and clients in March 2018, if successful.
Project status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Key dates
- Project start: February 2017
- Diagnostics: March – May 2017
- Solution design: June – August 2017
- Initial pilot: September 2017 – February 2018
- Full implementation: March 2018 – October 2018
- Project evaluation: February – October 2018
Implementation sites
St George Community Mental Health Service, South Eastern Sydney Local Health District
Partnerships
Centre for Healthcare Redesign
Evaluation
The process of nursing staff meeting with clients and attending the clinical review did not occur as planned, due to an outbreak of norovirus followed by influenza that closed the ward. This made it difficult to have the same two nurses provide care for the consultant psychiatrist’s clients. Despite this setback, nurses attended 50 per cent of clinical reviews as of November 2017, which is an improvement on the pre-implementation rate of zero per cent.
As of November 2017, results indicate that the new model of care has improved staff and client satisfaction, reduced readmission rates, increased client engagement with community clinicians and increased the number of discharge plans developed in consultation with the client. A full evaluation will be conducted from February to October 2018, which will measure the following outcomes:
- St George Acute MHU readmission rates within 28 days of discharge
- percentage of readmissions from active community clients who had no contact with a community clinician
- percentage of readmissions from newly-referred community clients who had no contact with a community clinician
- percentage of clients in the MHU who believe they were included in decisions about their treatment and discharge planning
- percentage of clinical review meetings where the consultant psychiatrist provided a specific time and attended
- percentage of clinical review meetings where the nursing staff attended with the consultant psychiatrist
- percentage of community clients who had contact with their clinician while in the MHU within 72 hours of admission
- percentage of newly-referred community clients in the MHU who were seen by their community clinician within 72 hours of referral.
Lessons learnt
- Ongoing communication and feedback with all stakeholders is critical to the success of the project.
- Projects often take more time than anticipated. If completed within work hours, two full days per week is required up until the implementation phase.
- It is important to find a project sponsor who is approachable and available during the course of the project.
- To increase the chances of success, make adjustments to ensure the project meets the frame of reference.
- Be clear about what is being changes and why, as well as the desired outcomes and benefits.
- Remember that the project can only succeed with the cooperation and support of people who have the ability to create long-term change (change agents).
Contacts
Jeanine Smith
Community Service Manager
St George Mental Health
South Eastern Sydney Local Health District
Phone: 02 9553 2500
Jeanine.smith@health.nsw.gov.au