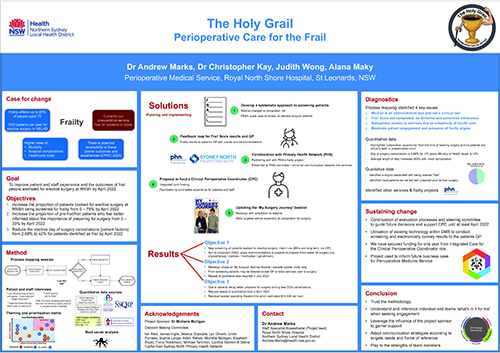
This project seeks to screen all patients on the elective surgical waitlist for frailty and optimise the health of those who are frail prior to their surgery. Five solutions were co-designed and are currently being implemented to allow a systematic screening for frailty and support the patient as they prepare for their surgery.
View a poster from the Centre for Healthcare Redesign graduation December 2021.
Aim
Our goal is to improve patient and staff experience and the outcomes of frail people waitlisted for elective surgery at Royal North Shore Hospital (RNSH) by April 2022.
Objectives
- Increase the proportion of patients booked for elective surgery at RNSH being screened for frailty from 0 to 75% by April 2022.
- Increase the proportion of pre-frail or frail patients who feel better informed about the importance of preparing for their surgery from 0 to 33% by April 2022.
- Reduce the elective day of surgery cancellations from patient factors from 2.68% to ≤2% for patients identified as frail by April 2022.
Benefits
- All surgical patients are screened for frailty and can opt in to receive communication of their frailty screen.
- Patients can dedicate their waiting time for surgery and turn it into their preparation time with support from the clinical perioperative coordinator.
- All patients are provided with opportunities and awareness of best practice preparation for surgery.
- The patient’s general practitioner is better informed about the patient’s frailty status.
- Staff benefit from support and knowledge sharing by the clinical perioperative coordinator.
- There are opportunities for greater cohesion and communication between clinicians involved in patient’s perioperative care.
- Patients receive assistance with case management.
- The hospital and district gain frailty data (previously uncollected).
- Opportunity for project to inform the development of the perioperative medicine service.
Background
Frailty is a syndrome of physiological decline, characterised by a marked vulnerability to adverse health outcomes.1 Perioperative frailty doubles the risk of surgical complications and adverse outcomes, such as falls, fractures and loss of independence, and may lead to increased length of stay and increased mortality.2,3
Frailty affects up to 25% of people aged over 70 years of age.4 40% of people in this same age group are also pre-frail.4 Northern Sydney Local Health District has an ageing population and by 2026, our population over 70 years will have increased by 34%.5 This equates to over 1000 patients a year who present for elective surgery in Northern Sydney Local Health District each year.
Despite frailty affecting so many people, RNSH has yet to screen and treat frailty in our elective surgical patients. This means that both patients and clinicians are not aware of their frailty and its related adverse outcomes. In older surgical patients, the prevalence of frailty can be as high as 50%.6
The waiting time for elective surgery at RNSH can range from 12 days to 239 days. Currently, this time is a missed opportunity to better prepare our frail elective surgery patients prior to their surgery.
Implementation
Initiation
We completed the following activities to help us understand our context, setting and problem.
- Conducted a literature review on frailty prevalence and impacts on post-operative recovery
- Conducted a literature review on management and reversibility of frailty
- Wrote an Aboriginal Health Impact Statement
- Created a steering committee (Frailty Decision Making Committee)
- Wrote our project management plan. This included a stakeholder map, communications plan and Gantt chart.
Diagnostics
We analysed the current journey of the RNSH elective surgical patient through three broad categories:
- process mapping
- qualitative research
- quantitative research.
Process mapping was completed through a workshop that included all the key stakeholders involved in the booking patients for pre-admission clinics and surgery, screening the patients, and admitting patients for surgery.
Qualitative research included:
- conducting patient interviews to write patient stories
- conducting staff interviews at RNSH and throughout the district
- analysing complaints using our incidents and complaints management system
- conducting a patient survey in the community.
Quantitative research included:
- looking at variety of data bases, such as National Surgical Quality Improvement Program, RNSH datasets and Health Round Table.
- comparing data points, such as day of surgery cancellation, average waitlist timeframes, average length of stay, post-operative complications and hospital acquired complications.
We consolidated all our findings into 14 main themes. The Frailty Decision Making Committee then prioritised our top four themes based on our ability to influence them and the impact on project objectives.
- Frailty screening is not currently completed.
- Waitlist is an administrative tool and not used for clinical purposes.
- Limited patient engagement and the presence of frailty stigma.
- Patients cannot access services due to the complexity of the healthcare system.
- Root causes analysis (five whys) was conducted to determine the root causes to each issue. This was the basis for the development of our solutions.
Solutions
We consulted with our key stakeholders, including patients, again to co-design our five solutions.
- Develop a systematic approach to screening patients for frailty using the FRAIL Scale7.
- Create a clinical perioperative coordinator role.
- Create a feedback loop of the FRAIL scale results for each patient’s general practitioner.
- Partner with the Sydney North Primary Health Network to create a frailty optimisation pathway.
- Update the My Surgery Journey patient education booklet to better inform patients about frailty, its impact on post-operative recovery and its reversibility.
Implementation
As of mid-July 2021, we have started the following aspects of the implementation.
- Patients are screened and this is documented this in our electronic medical record system. The phone call to the patient consists of a frailty screen, generic advice on benefits of preparing for surgery and directions to the My Surgery Journey website or sending them a booklet.
- Funding to support the clinical perioperative coordinator position was approved.
The clinical perioperative coordinator will take responsibility for screening, care coordination and health optimisation of our frail elective surgery patients. - The FRAIL scale results are sent to the general practitioner of each patient we’ve screened.
Audit of eight general practitioner letters was conducted by phoning the general practices. The letters were not being sent electronically. This was an unknown error and has been escalated to the information technology team to address. The team are using an alternative process to send the letter until an embedded solution is achieved. - Maintaining communication channels with the Primary Health Network in order to co-create an optimisation pathway.
Joint agreement was signed to share data on an ongoing basis at Frailty Decision Making Committee.
Initial data presented by Primary Health Network in October 2021 revealed top interventions prescribed for frailty by general practitioners were physiotherapy (40%) and healthy lifestyle group exercises (19%). - New sections on preparing for surgery and education about reversing effects of frailty added to the My Surgery Journey booklet. Additional revision of booklet conducted with input from subject matter experts. The updated draft of the My Surgery Journey patient education booklet has been approved by RNSH and district stakeholders.
The Frailty Decision Making Committee will continue beyond February 2022 for at least another six months in order to provide support and accountability for our proposed solutions. The Frailty Decision Making Committee will disband once all these solutions have become business as usual and oversight will be maintained by the division of surgery and anaesthesia.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- Initiation: 16/2/21 – 22/3/21
- Diagnostics: 23/3/21 – 18/5/21
- Solutions: 18/5/21 – 20/7/21
- Implementation: 21/7/21 – 26/8/21
- Sustainability: 27/8/21 – 18/2/22
Implementation site
Royal North Shore Hospital, Division of Surgery and Anaesthesia
Partnerships
- Centre for Healthcare Redesign
- Sydney North Primary Healthcare Network
Results
Solution 1: Develop systematic process of screening elective surgical patients for frailty
- Screening started on 13 July 2021
- To date, we have screened 98 patients, of which 44 (45%) were pre-frail or frail.
- Evaluation of the phone call occurred within the same session – patients were asked if they found the phone call helpful.
- 41 (93%) of the pre-frail or frail patients found the screening phone call helpful.
- Even some patients who were not frail found these screening phone calls helpful.
Solution 2: Submit a proposal to fund the clinical perioperative coordinator
We are working closely with RNSH finance and performance teams to quantify the work done by the clinical perioperative coordinator. The supporting data and costing analysis will feed into a benefits realisation plan, which will be used to help secure a permanent source of funding.
Solution 3: Create a feedback loop of the FRAIL scale results for each patient’s general practitioner
We are aiming for a letter received rate of 95%. We will complete random audits on GP practices on whether the FRAIL scale results letter was received. This will be done via a phone call. Due to patient confidentiality, we will not be able to ask the GP if they were actioning any of the recommendations for their patient.
Solution 4: Partner with the Sydney North Primary Health Network to create a frailty optimisation pathway
This will be viewed as a success when GPs collaborate with the clinical perioperative consultant by identifying their frail patients needing elective surgery at Royal North Shore Hospital.
Solution 5: Update the My Surgery Journey patient education booklet
Evaluation of the My Surgery Journey website will be evaluated by the number of visits to the website and the number of printed copies requested.
Lessons learnt
- Trust the methodology.
- We would do Redesign School again – the structured method was very helpful.
- Always test your assumptions.
- Test and re-test solutions.
- Consumer input is vital.
- Sponsorship has been key to our success. Sponsors have driven engagement with key stakeholders and have expressed, modelled and reinforced expectations.
References
- Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet. 2013 Mar 2;381(9868):752-62. DOI: 10.1016/S0140-6736(12)62167
- Darvall JN, Loth J, Bose T, et al. Accuracy of the Clinical Frailty Scale for perioperative frailty screening: a prospective observational study. Can J Anaesth. 2020;67(6):694-705. DOI:10.1007/s12630-020-01610-x
- Hall DE, Arya S, Schmid KK, et al. Association of a frailty screening initiative with postoperative survival at 30, 180, and 365 days. JAMA Surg. 2017;152(3):233-40. DOI:10.1001/jamasurg.2016.4219
- Thompson MQ, Theou O, Karnon J, et al. Frailty prevalence in Australia: Findings from four pooled Australian cohort studies. Australas J Ageing. 2018;37(2):155-58. DOI:10.1111/ajag.12483
- Northern Sydney Local Health District. Clinical Services Plan 2019- 2022. Sydney: Northern Sydney Local Health District; 2019.
- Partridge JS, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing. 2012;41(2):142-47. DOI:10.1093/ageing/afr182
- Woo J, Leung J, Morley JE. Comparison of frailty indicators based on clinical phenotype and the multiple deficit approach in predicting mortality and physical limitation. Journal of the American Geriatrics Society. 2012 Aug;60(8):1478-1486. DOI: 10.1111/j.1532-5415.2012.04074.x
Contacts
Dr Andrew Marks
Staff Specialist Anaesthetist (Project lead)
Royal North Shore Hospital
Northern Sydney Local Health District
Andrew.Marks@health.nsw.gov.au
Alana Maky
Registered Nurse
Royal North Shore Hospital
Northern Sydney Local Health District
Alanakay.Maky@health.nsw.gov.au
Judith Wong
A/ Service Improvement Manager, Senior Orthopaedic Physiotherapist
Royal North Shore Hospital
Northern Sydney Local Health District
Hangwah.Wong@health.nsw.gov.au
Dr Chris Kay
Anaesthetics Fellow
Royal North Shore Hospital
Northern Sydney Local Health District
Christopher.Kay@health.nsw.gov.au