This project utilises Clinical Redesign Methodology in a multifaceted approach to prevent post-operative urinary tract infections in our Network.
Aim
By the end of 2020 we will reduce the urinary tract infection rates in the Sydney Children’s Hospital Network by 50% from baseline 2018 data.
Benefits
- Improve patient outcomes by preventing post-operative urinary tract infections.
- Reduce costs and length of stay due to post-operative urinary tract infections.
- Improve clinical staff confidence and knowledge regarding urinary catheters.
- Improve parent/carer experience in caring for their child post-operatively.
- Reduce median time catheter in situ.
Program status
Program dates
The Project commenced in April 2019 and will conclude in December 2021. The milestones for the project are depicted below:
- Planning - April 2019
- Diagnostics - July 2019
- Solutions - August 2019
- Implementation - October 2019 - 2020
- Evaluation - 2020/2021
- Project end - 2021
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Background
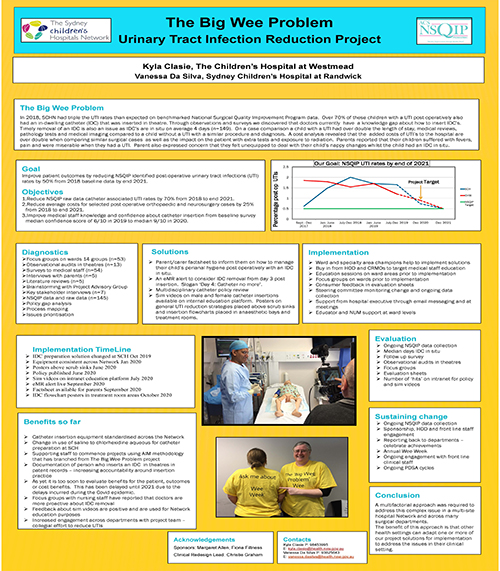
Our Network enrolled into the National Surgical Quality Program (NSQIP) in mid-2017. This Program collects data on post-operative complications along with the patient’s pre-operative condition and case complexity. This data is then statistically risk-adjusted and case-mix adjusted and benchmarked with >130 paediatric hospitals internationally. In 2018, the Sydney Children’s Hospital Network were over 3 times higher than expected when benchmarked internationally.
Parents were interviewed and they reported that they lacked confidence in how to care for their child after surgery if they had a urinary catheter inserted. They felt unsupported if their child had soiled their nappy and required perianal hygiene. They shared that ‘they did the best that they could’ but were not sure the cleanliness of the catheter was adequate. They reported that their child had extra tests, longer length of stay and that they had disrupted sleep due to comforting their child whilst they were experiencing symptoms as a result of the urinary tract infection.
The medical staff were sent surveys asking them to rate their confidence in inserting a catheter. They rated themselves with a median 6/10 confidence score. We also performed observational audits in theatres of medical staff inserting urinary catheters and found that 11 out of 13 audits were non-compliant with hospital policy.
We performed 14 semi-structured focus groups in clinical areas and discovered some themes. These themes were communication issues, lack of daily perianal hygiene, catheter troubleshooting and ambiguity in the hospital policy. A policy gap analysis was performed which uncovered that large sections were missing or lacking in detail.
We formed a Project Advisory Group and process mapped the impact of urinary catheterisation on a child throughout their surgical admission. We mapped the issues in a fishbone diagram and from there we prioritised them. We performed literature reviews to inform us of best practice and possible solutions moving forward.
We performed 145 chart reviews of surgical patients with a urinary catheter inserted in theatres. The median days of a catheter in situ was 4 days in 2018. From our literature search we found that best practice is to remove urinary catheters by day 3 where possible.
Implementation
Solution design and implementation was staggered to maximise success due to multiple conflicting demands being experienced across the Sydney Children’s Hospitals Network.
Solutions for implementation are as follows:
- Education Package:
- Simulation video for medical and nursing staff on the insertion of an indwelling catheter.
- Posters outlining correct procedural steps for indwelling catheter insertion for treatment areas.
- Posters in operating theatres to discourage unnecessary insertion of indwelling catheters.
Status: Video and Posters have been designed and completed. Used for education purposes for medical and nursing staff.
- Parent Involvement Package:
- Indwelling catheter factsheet for parents and carers highlighting important information regarding the indwelling catheter and necessary cares.
- Consumer engagement through parent and carer interviews to help inform the content of the factsheet.
Status: Factsheet published and available for use in ward areas.
- Indwelling Catheter removal flagging system on electronic Medical Records (eMR):
- eMR alert developed to prompt nurses and doctors to review need for catheter.
Status: eMR flagging system developed and implemented.
- Policy review and update:
- Multidisciplinary review of the current Network indwelling catheter policy.
- Utilising current literature and evidence based practice relevant to all stages of indwelling catheter insertion and care.
Status: Policy published, reviewed twice with feedback and education given about updated policy.
Implementation was delayed due to the current COVID-19 pandemic.
Implementation sites
- Sydney Children’s Hospital Network
- The Children’s Hospital at Westmead
- The Sydney Children’s Hospital
Partnerships
- Centre for Healthcare Redesign
- Agency of Clinical Innovation
- University of Tasmania
- National Surgical Quality Improvement Program – American College of Surgeons
Results
Overall evaluation is achieved through our National Surgical Quality Program six monthly data reports of our benchmarked post-operative complication rates.
Solution 1: Education Package (Sim videos and posters)
Measure with observational theatre audits and repeat survey to medical staff at end 2020. Evaluation sheets after education sessions in clinical ward areas. Measure amount of ‘hits’ on video platform.
Solution 2: Parent Involvement Package (Factsheets)
Evaluation sheets with factsheet for parents/carers. Interviews with parents/carers and focus groups with nursing staff feedback. These evaluations will occur end of 2020 after solution roll out.
Solution 3: Urinary catheter removal flag
Median days catheter in situ monitored in chart reviews. Electronic medical record reports of length of time catheters are in situ. These will occur at the end of 2020 after the removal flag rollout in August 2020.
Solution 4: Multidisciplinary team Urinary Catheter Policy review
Policy available on Network ePolicy platform. Number of ‘hits’ on the policy monitored through ePolicy platform at end 2020.
Lessons learnt
- Define project scope during all levels of the project.
- Focus on one to two ‘big ‘solutions or no more than three to four smaller solutions.
- Engage with sponsors on a regular basis and keep them informed and involved as much as possible throughout the whole process.
- During the project remember to refer to the stakeholder map regularly.
- Address issues and risks early to minimise the impact to the project.
References
- Fukoka, et al (2018) Longer duration of urinary catheterization increases catheter-associated urinary tract infection in PICU. Paediatric Critical Care Medicine, 19(10): E547–E550
Further Reading
Contacts
Vanessa Da Silva
Surgical Clinical Reviewer
Sydney Children’s Hospital at Randwick
Phone: 02 9382 5643
Vanessa.DaSilva@health.nsw.gov.au
Kyla Clasie
Surgical Clinical Reviewer
The Children’s Hospital at Westmead
Phone: 02 9845 3995
Kyla.Clasie@health.nsw.gov.au