This project aims to provide proactive care for heart failure patients in the Hunter New England Local Health District (HNELHD). It will support people with heart failure who are transitioning from hospital to home and back into the ongoing care of their general practitioner (GP).
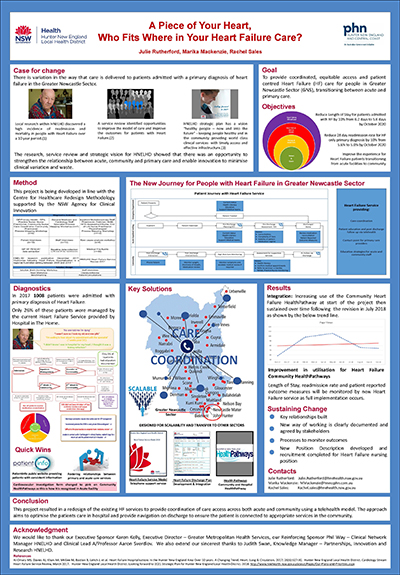
View a poster from the Centre for Healthcare Redesign graduation, December 2018.
Aim
- To provide equitable, coordinated, and patient-centred heart failure (HF) care for people in the Greater Newcastle Sector (GNS), who are transitioning between acute and primary care.
- To improve the experience for HF patients transitioning from acute facilities to primary care by increasing access to a HF service from 26% to 36.4% by October 2019.
- To reduce the 28 day readmission rate for people with HF by 10% from 9.7% to 8.7% by October 2020.
- To reduce length of stay for patients admitted with HF by 10% from 8.3 days to 7.5 days by October 2020.
Benefits
- Improved collaboration between the Hunter New England and Central Coast Primary Health Network and HNELHD .
- Reduced clinical variation, leading to improved support for clinical decision making.
- Increased access and equity in service provision.
- Improved quality of life for patients.
- More efficient use of finite resources.
- Enhanced support for people with HF on the end of life care journey.
Background
An increase in the HF population over the past 10 years has increased demand on the HF service in HNELHD .1
Currently in the GNS , Hospital in the Home offers specific HF care as an inpatient model. In 2017, 1008 patients in the GNS were admitted with a primary diagnosis of HF . Of those admitted patients 26% were managed by the current HF specific service based within Hospital in the Home – a 74% variation from the recommended standard of care. This variation has the potential to impact patient outcomes including readmission and all-cause mortality.
Patients and clinical staff identified a fragmented journey from hospital to discharge to primary care. During the diagnostic phase, our HF patients reported that they didn’t understand changes to their medications, were unclear on their diagnosis or the trajectory of their disease, and that they had difficulty navigating the health care system once discharged from hospital.
Primary care clinical staff discussed delays in delivery of care to patients due to difficulty arranging timely specialist and outpatient investigative reviews; discharge summaries did not provide a clear action plan for medication titration or follow up requirements; the process to discuss end of life and/or palliative care referrals was also unclear.
Implementation
The following three solutions are in the implementation phase.
- Redesign the HF service model for the GNS to provide a central point of contact for patients, specialist services and primary care. There are three main functions of the new service design.
- Liaison with acute care staff to ensure evidence-based care during a hospital admission and on transition of care.
- Use of telephone management to coordinate post discharge care for all HF patients according to their needs.
- Provision of a central point of contact to support GPs and practice nurses and build capacity in primary health care to better manage patients with HF .
- Development of HealthPathways (HP) suite to support HF management
- Implementation and communication of HF Community HealthPathway (CHP), articulating clear referral processes from primary care to acute services, guiding evidence based clinical management for primary care, defining appropriate points of care for referral to palliative care, and assisting with end of life discussions has been completed. A practice nurse resource page is in development.
- PatientInfo public website to host endorsed patient related information relating to HF at an appropriate health literacy level to be viewed outside of a clinical consultation. Patient information will be consistent between primary, outpatient and inpatient settings- achieved
- Development of a HF HHP (Hospital HealthPathway) articulating acute assessment, management and referral in line with HNELHD Policy Procedure Guidelines. HFHHP soft-launch achieved. Hard launch and implementation activities are scheduled for mid-December 2018.
- Heart Failure Discharge Plan Checklist developed, and in implementation phase to:
- promote patient safety through improved clinical handover between acute and primary care providers
- provide a clear action plan for GP interventions including end of life discussions
- clearly communicate medication changes to the GP with guidance for titration of medical therapy
- provide clarity to the patient and GP around self-management hyperlinking to the patient resources on HealthPathways and PatientInfo.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- 15-22 August 2018: conducted HF service model testing.
- November 2018: commence service model pilot, following recruitment of HF nurse.
- July 2019: evaluation of service model following pilot period.
Implementation sites
The service model will initially be implemented in the GNS with the John Hunter Hospital being the initial pilot site. The Hospital HealthPathways is scheduled for hard launch in mid-December 2018, with the Discharge Plan Checklist template piloting in January 2019.
Partnerships
Hunter New England Local Health District - Heart Failure project is supported by the Centre for Healthcare Redesign, and Hunter New England Central Coast Primary Health Network.
Evaluation
Baseline measures have been obtained and evaluation is scheduled to commence in July 2019.
Solution 1 - Redesigning the service model
Short to medium data collection on referrals to service, clinical service interventions. For example, data on palliative care referrals, medication reconciliation, patient reported outcome measures - completion of Kansas City Cardiomyopathy Questionnaires, and clinician and patient feedback. Long term key performing indicators include reduction in length of stay and 28 day readmission reports.
Solution 2 - HealthPathways
Short to medium data collection of google analytics including; page views, audience behaviour and session length regarding HHPs , CHPs and practice nurse resource page. Use of PatientInfo website. Long term key performing indicators include reduction in length of stay and 28 day readmission reports.
Solution 3 - HF discharge plan checklist
Short to medium data collection from auditing medical health records on utilisation rates, and clinician feedback. Long term key performing indicators include reduction in length of stay and 28 day readmission reports.
Lessons learnt
For this large scale redesign project, multiple team members, with varying expertise have been pivotal. Key lessons include:
- the importance of good time management
- secure trust by establishing a communication plan and risk and issues registry
- clearly define the change, explain what is changing and the consequences of not changing. This provides a compelling case for change and greatly assists in managing change and expectations.
- consultation and collaboration with key stakeholders to maintain a clear and structured approach provides consistency among clinicians - involve people early
- be realistic and consider workplace culture
- maintain sponsor and clinical lead commitment to achieve buy-in and assist with leverage, identifying weak spots and developing solutions to mitigate risk.
References
- Al-Omary MS, Davies AJ, Khan AA, et al. Heart Failure Hospitalisations in the Hunter New England Area Over 10 years. A Changing Trend. Heart, Lung & Circulation. 2017; 26(6):627-30.
Further reading
- Atherton JJ, Sindone A, De Pasquale CG, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Guidelines for the Prevention, Detection, and Management of Heart Failure in Australia 2018. Heart, Lung and Circulation. 2018; 27(10):1123-208.
- ACI Cardiac Network. NSW clinical service framework for chronic heart failure 2016. Chatswood NSW: NSW Agency for Clinical Innovation; 2017.
- Krum H, Forbes A, Yallop J, et al. Telephone support to rural and remote patients with heart failure: the Chronic Heart Failure Assessment by Telephone (CHAT) study. Cardiovasc Ther. 2013; 31(4):230-7.
- Taylor CJ. Management of chronic heart failure in general practice in Australia. Australian family physician.45 (11):823-7.
- Huynh Q, Negishi K, De Pasquale C, Hare J, Leung D, Stanton T, et al. Effects of post-discharge management on rates of early re-admission and death after hospitalisation for heart failure. Med J Aust. 2018; 208(11):485-91.
- Hesselink G, Schoonhoven L, Plas M, et al. Quality and safety of hospital discharge: A study on experiences and perceptions of patients, relatives and care providers. International Journal for Quality in Health Care. 2013; 25(1):66-74.
- Riley JP, Masters J. Practical multidisciplinary approaches to heart failure management for improved patient outcome. European Heart Journal Supplements. 2016; 18(suppl_G):G43-G52.
- Inglis SC, Clark RA, McAlister FA, et al. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: Abridged Cochrane Review. European Journal of Heart Failure. 2014; 13(9):1028-40.
- Flodgren G, Rachas A, Farmer AJ, et al. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews. 2015(9).
- Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125(9):915-21.
- Slyer JT, Concert CM, Eusebio AM, et al. A systematic review of the effectiveness of nurse coordinated transitioning of care on readmission rates for patients with heart failure. JBI Libr Syst Rev. 2011;9(15):464-90.
- Branowicki PM, Vessey JA, Graham DA, et al. Meta-Analysis of Clinical Trials That Evaluate the Effectiveness of Hospital-Initiated Postdischarge Interventions on Hospital Readmission. Journal For Healthcare Quality November/December. 2017;39(6):354-66.
- Inglis SC, Clark RA, Dierckx R, et al. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst Rev. 2015(10):Cd007228.
- Jayakody A, Bryant J, Carey M, et al. Effectiveness of interventions utilising telephone follow up in reducing hospital readmission within 30 days for individuals with chronic disease: a systematic review. BMC Health Serv Res. 2016; 16(1):403.
- Cherofsky N, Onua E, Sawo D, et al. Telehealth in adult patients with congestive heart failure in long term home health care: a systematic review. JBI Libr Syst Rev. 2011; 9(30):1271-96.
- Spinsante, S. Home telehealth in older patients with heart failure- costs, adherence, and outcomes. Smart Homecare Technology and Telehealth. 2014; 2014(default):93-104.
Contact
Julie Rutherford
Heart Failure Project Manager
Hunter New England Local Health District
julie.rutherford@hnehealth.nsw.gov.au