Wollongong Hospital (WH) implemented a program to optimise the pre-operative haemoglobin and iron stores of patients undergoing major elective colorectal, upper GIT and orthopaedic surgery. This will prevent avoidable blood transfusions and their complications, along the patient peri-operative journey.
View a poster from the Centre for Healthcare Redesign graduation, August 2018.
Aim
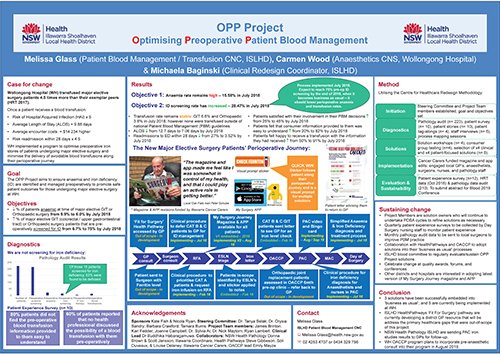
To decrease the rate of patients who are anaemic at the time of major surgery from 9.9% to 6.0% by July 2018.
To increase the rate of patients that are screened pre-operatively for iron deficiency (ID) from 6.7% to 75% by July 2018.
Benefits
Patients
- Receive consistent, easy to understand, information throughout the pre-operative journey.
- Participate in patient blood management (PBM) decisions.
- Receive timely treatment for anaemia and iron deficiency before major elective surgery.
- Avoid preventable transfusions and potential complications.
Staff
- Multidisciplinary collaboration between general practitioners (GPs), surgeons, anaesthetists, perioperative service nurses, and medical ambulatory care service nurses.
- Deliver timely multimodal PBM to optimise patients for surgery.
Healthcare system
- Support multidisciplinary collaboration.
- Reduced costs related to avoidable transfusion (additional encounter cost; longer length of stay; higher rates of hospital acquired infections, and higher rates of readmission).
Background
In Australia, over 4.5% of the population is at risk of anaemia. Women are at a higher risk (6.4%) than men (2.5%), and the risk rapidly increases after the age of 65 years.1 Its prevalence and impact is similar to diabetes and cardiovascular disease.2 Anaemia, defined as having an insufficient circulating mass of red blood cells resulting in low levels of haemoglobin (< 130g/L in males; and <120g/L in females), impacts the body’s ability to oxygenate tissues and organs.3-4 Even in mild forms, it can lead to impaired function and reduced quality of life.4 Prevalence in surgical patients is generally 20-40%, but higher (60%) in colorectal surgery populations.4 Iron deficiency is the most prevalent nutritional deficiency in the world and the most common cause of anaemia in surgical patients.5-6
Benchmarked case-mix and pathology data indicated that WH’s transfusion rate was 4.5 times their exemplar peer hospital’s rate in 2016.7 A retrospective audit of 223 WH major elective orthopaedic, upper gastrointestinal and colorectal surgery patients revealed that only 10% of patients were anaemic preoperatively, which is significantly lower than the claimed prevalence of preoperative anaemia in higher income countries (28.7%-30.4%) in the literature.8 However, 93.3% of the cohort was not screened for ID. Of those who were screened, 53% were diagnosed, or likely, iron deficient. Since it is possible to be iron deficient without anaemia, and inadequate iron stores or availability can limit postoperative erythropoiesis, WH’s high transfusion rate in major elective surgery patients could be partly attributable to a high incidence of undiagnosed and untreated ID. As such, this makes for a strong case to provide optimal preoperative anaemia and ID management.
Preoperative anaemia and ID may lead to treatment with perioperative blood transfusion, however transfusion can increase the risk of longer hospital stay, surgical complications, and increased mortality.9 Patients that received transfusion in the WH major elective surgery cohort were five times more likely to acquire an infection; stayed on average nine days longer; and were 4.5 times more likely to re-admit within 28 days of discharge.10
Elective surgery patients and healthcare providers (GPs, surgeons, anaesthetists, and nurses) were interviewed to investigate why patients are not optimised while they await planned major surgical procedures. A significant finding of these interviews was that the patient journey is complex and involves numerous stakeholders. The key issues that WH perioperative service identified and had influence over were:
- no process for patients to be routinely screened and treated for iron deficiency
- patients and their carers were not empowered with adequate information; or encouraged to collaborate with their healthcare providers.
Implementation
Root causes
- No system prompt for iron studies or ferritin.
- No local guideline for prompting optimal pre-operative PBM targets (including adequate iron stores) for major elective surgery.
- Written information provided to patients is very general and does not offer possible alternatives to perioperative PBM transfusion.
- No specific perioperative PBM care plan available to prompt staff to offer optimal PBM and involve patients in their plan of care.
- Low level of collaboration between the primary health network and perioperative service.
Solutions
- Elective surgery waitlist nurse identification of major elective surgery patients requiring PBM screening using the ‘Check Ferritin’ sticker
- Category 2 (surgery scheduled <90 days) colorectal and upper GIT patients are sent a letter to return to GP for iron level check
- Orthopaedic joint replacement patients are to be captured in OACCP clinic by anaesthetists (at six month visit) pathology testing done and patient sent back to GP for management
- Category 1 (surgery scheduled <30 days) are to have ambulatory care clinic priority for iron infusions:
- Surgeons to flag on request for admission form
- Elective surgery waitlist nurse to check surgeon has referred and prescribed treatment
- Clinical guideline and treatment algorithm and procedure for managing pre-operative anaemia and/or iron deficiency to include:
- Ambulatory care clinic referral process for Anaesthetists who diagnose deficiency in pre-admission clinic
- Collaboration with ISLHD Health Pathways and Coordinare to link into holistic ‘Fitness for Surgery’ pathway for GPs
- Linking to ISLHD administration of Ferrous Carboymaltose (Ferinject®) procedure
- Routine iron studies on major elective surgery patients in pre-admission clinic
- Collaboration with NSW health pathology and ISLHD pathology staff to ensure copies of results are provided to GPs
- My Surgery APP edited to include blood optimisation, conservation, and transfusion information:
- Iron animation
- My Surgery Journey Magazine edited to include blood optimisation, conservation, and transfusion information
- Pre-admission clinic bingo card empowering patients to start PBM conversations with their healthcare providers, and ensure they are involved in their PBM plan of care
- Pre-admission clinic video delivering unit specific information for patients including PBM content
Status
Implementation – The project is currently being implemented.
Dates
- Application commenced 1 February 2018
- Project commenced 18 July 2017
- Evaluation completed 31 August 2018
Implementation sites
Colorectal, Upper Gastrointestinal and Orthopaedic surgery at Wollongong Hospital, Division of Surgery, ISLHD
Partnerships
- Centre for Healthcare Redesign
- New South Wales Health Pathology
- New South Wales Health Pathology - ISLHD
- HealthPathways - Illawarra Shoalhaven
- Coordinare – South Eastern New South Wales
Results
Retrospective pathology and patient file audit (n=210) of all major elective colorectal, upper GIT and orthopaedic procedures May-July 2018; and patient experience surveys (n=12) in August 2018 evaluated.
Objectives
- Anaemia rate increased from 9.9% to 15.58% by July 2018 (target was 6.0%)
- ID screening rate has increased from 6.7% to 28.47% by July 2018 (target was 75%)
- A routine procedure for pre-operative ID screening was only implemented in July 2018. We expect to reach the target of 75% by the end of 2018, when the process becomes business as usual – which we expect to lower the perioperative rates of anaemia and transfusion.
Benefits
- Transfusion rate remains stable: GIT 6.6% and Orthopaedic 3.8 in July 2018, however none were transfused outside of national Patient Blood Management guidelines.
- Average length of stay decreased from 12.7 days to 7.1 days by July 2018
- Re-admissions to the emergency department within 28 days decreased from 27% to 3.5% by July 2018
- Number of patients satisfied with their involvement in their PBM decisions increased from 25% to 45% by July 2018
- Number of patients who felt that information provided to them was easy to understand increased from 20% to 82% by July 2018
- Number of patients who felt happy to receive a transfusion with the information they had received grew from 50% to 91% by July 2018
Additional benefits such as the potential for a decrease in average total encounter cost, and hospital acquired infections will be evaluated from case-mix data from the finance department and health roundtable (available in December 2018).
Lessons learnt
- Ongoing sponsorship is vital to the individual success of each solution – don’t forget to keep your sponsor well-briefed and engaged throughout the project. They won’t know how to help you unless you tell them what you need.
- Maintaining a strong commitment from the steering committee and project team members ensures a project stays on track.
- Prepare for ongoing resource barriers for solutions – be creative and consider external funding sources to ensure you can proceed with your solutions
- Doing the redesign project without backfill of substantive positions will disrupt project momentum - recruit a project officer and backfill before commencing the project.
References
- Australian Bureau of Statistics. Australian Health Survey: Biomedical Results for Chronic Diseases, 2011-12. Canberra: ABS; 2013. 45p. Cat. no. 4364.0.55.005. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.005Chapter7002011-12
- Partridge J, Harari D, Gossage J, et al. Anaemia in the older surgical patient: a review of prevalence, causes, implications and management. J R Soc Med. 2013 Jul;106(7):269-77.
- World Health Organisation. Nutritional Anaemias: Report of a WHO Scientific Group. Geneva: World Health Organisation; 1968. 40p. Report No.: 405. Available from: http://apps.who.int/iris/bitstream/handle/10665/40707/WHO_TRS_405.pdf?sequence=1&isAllowed=y
- Clevenger B, Mallett SV, Klein AA, et al. Patient blood management to reduce surgical risk. Br J Surg. 2015 Oct; 102(11):1325-37. DOI: 10.1002/bjs.9898.
- Shander A, Van Aken, H, Colomina MJ, et al. Patient blood management in Europe. Br J Anaesth. 2012 Jul; 109(1) 55-68. DOI: 10.1093/bja/aes139.
- Kumar A, Auron M, Ereth M. Blood Management. Anaesth Clin. 2013; 31(2):316-21.
- Health Round Table. Patient Blood Management – Inpatient Analysis: Jan 2016-Dec 2016. Sydney: Health Round Table; 2017. 40p. Report No.: v01.
- Clevenger B, Richard T. Pre-operative anaemia. Anaesth. 2015 Dec; 70(1):20-8. DOI: 10.1111/anae.12918
- Ferraris VA, Davenport DL, Saha SP, et al. Surgical outcomes and transfusion of minimal amounts of blood in the operating room. Arch Surg. 2012 Jan; 147(1)49-55. DOI: 10.1001/archsurg.2011.790.
- Glass M, Wood C. Wollongong Hospital Optimising Preoperative Patient Blood Management Diagnostics Report. Wollongong: Illawarra Shoalhaven Local Hospital District; 2016. 1p. Report No.: 1.
Further reading
- National Safety and Quality Health Service: Standard 7 - Blood Management
- Bohlius J, Schmidlin K, Brilliant C, et al. Recombinant human erythropoiesis-stimulating agents and mortality in patients with cancer: a meta analysis of randomised trials. Lancet. 2009 May; 373(9674)1532-42. Available at: https://doi.org/10.1016/S0140-6736(09)60502-X
- Maxwell MJ, Wilson MJ. Complications of blood transfusion. Continuing Education in Anaesthesia, Critical Care & Pain. 2006 Dec; 6(6)225-9. Available at: https://doi.org/10.1093/bjaceaccp/mkl053
- Thomson A, Farmer S, Hofmann A, et al. Patient blood management – a new paradigm for transfusion medicine? ISBT Science Series 2009 Oct; 4(2)423–35.
Contact
Melissa Glass
Patient Blood Management / Transfusion Clinical Nurse Consultant
Illawarra Shoalhaven Local Hospital District
Phone: 0434 329 756
melissa.glass@health.nsw.gov.au