The Children’s Hospital at Westmead (CHW) is streamlining the referral, triage and booking processes to ensure timely access to magnetic resonance imaging (MRI) scans for paediatric patients. The project aims to positively impact the patient journey, improve health outcomes and the experience of patients, families and staff.
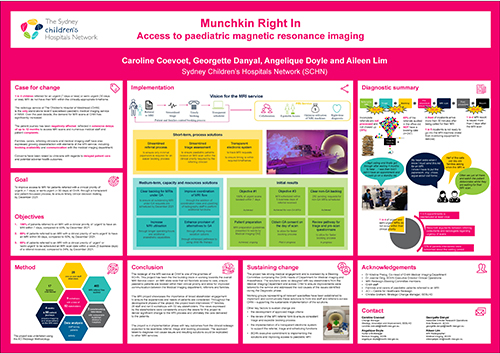
View a poster from the Centre for Healthcare Redesign graduation December 2021.
Aim
- Improve access to MRI for patients referred with a clinical priority of ‘urgent’ or ‘semi-urgent’ at CHW
- Develop a transparent and patient-focussed process
- Ensure timely clinical decision making.
Benefits
- Ensures timeliness of interventions and targeted treatments
- Improves health outcomes through timely diagnostic
- Improves the healthcare experience for children, parents and carers
- Enhances holistic approach to services delivery across the hospital
- Improves workplace culture and staff satisfaction.
Background
The radiology service at CHW is the only stand-alone level 6 specialised paediatric medical imaging service in NSW. Over the past decade, the demand for MRI scans at CHW has significantly increased. The patient journey has been negatively affected, reflected in extensive delays of up to twelve months to access MRI scans and numerous medical staff and patient complaints.
Families, carers, referring clinicians and medical imaging staff have also expressed growing dissatisfaction with elements of the MRI service, including booking availability and communication with the medical imaging department. Concerns have been raised by clinicians with regards to delayed patient care and potential adverse health outcomes.
MRI is a non-invasive imaging technique. To obtain a quality MRI scan, a patient must remain immobile for the duration of the scan (approximately 20-90 minutes depending on the number of sequences to be taken). To obtain the best possible images for children under the age of six, a general anaesthesia is usually required to provide immobility. Older children may be able to tolerate the MRI requirements, however may require longer appointment times or child-life therapy involvement in order to successfully have their MRI scan.1
CHW provides approximately 3,700 MRI scans to children each year. A third of these MRI scans are completed under general anaesthesia. Approximately 12% (two per day) are emergency unplanned MRIs.
Implementation
Extensive data audits, focus groups, interviews and surveys were conducted with staff and patient families to discover the root causes of the problem.
As of November 2021, the following solutions are in the process of being implemented.
- A simplified and streamlined referral process to ensure only minimal paperwork is required for an easier booking process.
- A standardised triage process to ensure paediatric patients receive an MRI scan within the clinical priority required by the referring clinician.
- A transparent electronic system where clinicians and medical imaging staff will be able to track MRI requests, receive automated notifications regarding their patient’s MRI appointment dates to ensure timing is within required timeframes.
- Timely communication between the medical imaging department and patients to ensure that families are aware of their appointment date, safety requirements of the MRI scanner and preparation for their scan.
- A new process to gather consent for MRI under general anaesthesia, where anaesthetists will obtain written consent for general anaesthesia on the day of the scan (currently this step is completed prior to the scheduling process).
- Regular education sessions on MRI patient preparation led by the medical imaging clinical nurse educator to be conducted with key CHW wards.
Other solutions have been identified and will be implemented once the above solutions are embedded into practices (expected mid to late 2022).
- Create two coordination roles within the medical imaging department to improve the daily operation of the department and the coordination of MRI patient flow.
- Upskill radiographers and nursing staff to cannulate and administer contrast (gadolinium) when required.
- Increase MRI operating hours and anaesthetic capabilities.
- Increase alternatives to general anaesthesia, such as sedation, as well as enhanced pathway to using child-life therapy capabilities.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
February 2021 to June 2022
Implementation sites
The Children’s Hospital at Westmead, Sydney Children’s Hospitals Network
Partnerships
Centre for Healthcare Redesign
Evaluation
As of November 2021, the project is in the early stage of implementation, with a pilot expected to start in mid-November 2021.
Process-improvement evaluation measures
- 100% of referrals are triaged within one business day
- 80% of MRI requests are allocated an appointment date within five business days
- 100% of patients referred to an MRI with a clinical priority of ‘urgent’ to have an MRI within seven days
- 80% of patients referred to an MRI with a clinical priority of ‘semi-urgent’ to have an MRI within 30 days.
Experience of care evaluation measures
- 80% of patients are called to select a suitable appointment date
- Survey of staff to measure staff satisfaction with the new process
- Survey of patients to measure improved patient experience
- Manual review of triaged referrals against triaged guidelines to ensure consistency.
Lessons learnt
- Consult broadly: seek input from all specialties and services accessing MRIs to ensure that all clinical priorities are addressed.
- Communicating for engagement and selecting communication strategies is critical to ensure buy-in from all stakeholders and keep the momentum.
- Keep it in perspective: the project exists to improve patient care and experience.
- Organisational support and endorsement are key to the success of each stage of the project.
References
- Pua EPK, Barton S, Williams K, et al. Individualised MRI training for paediatric neuroimaging: a child-focused approach. Dev Cogn Neurosci. 2020 Feb;41:1000750. DOI: 10.1016/j.dcn.2019.100750
Further reading
- Emery DJ, Forster AJ, Shojania KG, et al. Management of MRI wait lists in Canada. Healthc Policy. 2009;4(3):76-86.
- McGuirt D. Alternatives to sedation and general anesthesia in pediatric magnetic resonance imaging: a literature review. Radiol Technol. 2016 Sep/Oct;88(1):18-26.
- Paediatric Innovation, Education and Research Network Conference. Reducing the Need for General Anaesthetic through MR Play. [poster on internet]. 2018 [cited 29 October 2021]. Available from: https://www.piernetwork.org/uploads/4/7/8/1/47810883/mr_play_poster_v.final10.18.pdf
- Raschle N, Zuk J, Ortiz-Mantilla S, et al. Pediatric neuroimaging in early childhood and infancy: challenges and practical guidelines. Ann N Y Acad Sci. 2012;1252(1):43-50. DOI: 10.1111/j.1749-6632.2012.06457.x.
- Tokur S, Lederle K, Terris DD, et al. Process analysis to reduce MRI access time at a German University Hospital. Int J Qual Health Care. 2012;24(1):95-9. DOI: 10.1093/intqhc/mzr077
- Wessman BV, Moriarity AK, Ametlli V, et al. Reducing barriers to timely Magnetic Resonance Imaging scheduling. RadioGraphics. 2014;34:2064-70. DOI: 10.1148/rg.347140025
Contacts
Caroline Coevoet
Change Manager
South Eastern Sydney Local Health District
caroline.coevoet@health.nsw.gov.au
Georgette Danyal
Associate Director Research Operations
Sydney Children’s Hospitals Network
georgette.danyal@health.nsw.gov.au
Angelique Doyle
Nurse Unit Manager, Medical Imaging
Sydney Children’s Hospitals Network
angelique.doyle@health.nsw.gov.au
Aileen Lim
MRI Radiographer, Medical Imaging
Sydney Children’s Hospitals Network
aileenpeipei.lim@health.nsw.gov.au