Western Sydney Local Health District (WSLHD) established a Mental Health Acute Assessment Team (MHAAT) at Cumberland Hospital. The service responds to relevant Triple Zero calls via a dispatch system, using dedicated paramedics and mental health clinical nurse consultants.

Aim
To reduce inappropriate emergency department (ED) presentations by diverting Triple Zero calls from mental health consumers to specialist mental health clinicians.
Benefits
- Provides timely, appropriate and integrated care for mental health consumers.
- Reduces inappropriate ED presentations and bed block in hospitals.
- Improves assessment and referral capacity out of the hospital setting.
- Reduces demand on emergency and inpatient mental health services.
- Supports and develops the paramedic, police and healthcare workforce.
- Places specialist mental health clinicians on the frontline to de-escalate situations.
- Reduces stigma related to mental health by providing consumers with privacy, respect and a smoother transition to ongoing mental health care.
- Provides least restrictive mental health care options and empowers consumers to participate in their own management plan when appropriate.
Background
In 2013, the NSW Ministry of Health identified that 15 per cent of people who call Triple Zero for an ambulance require mental health care. Often these people were transported by paramedics to EDs for care, where they waited for an assessment and an acute bed in a designated mental health facility. It was determined that a new approach was required, to divert mental health care calls from Triple Zero to a service that could assess and refer mental health consumers to services outside the hospital setting.
Implementation
Cumberland Hospital implemented the new MHAAT service delivery model in 2013. The team responds to specified mental health calls to Triple Zero via a dispatch system, where a dedicated paramedic and mental health clinical nurse consultant partner up and attend to the emergency. The team provides a comprehensive medical and mental health assessment of the consumer on site.
If the assessment indicates that admission to a mental health facility is required, the mental health clinical nurse consultant can arrange a direct referral, rather than transporting the consumer to the hospital and forcing them to wait in the ED for a significant amount of time prior to admission. If the assessment indicates that the consumer can be cared for in the community setting, the consumer is directed to local services for treatment.
Status
Sustained – The project has been implemented and is sustained in standard business.
Dates
- November 2013 – MHAAT Trial Project Plan drafted
- December 2013 – Proof of Concept developed as a joint venture between WSLHD and NSW Ambulance Service
- June 2014 – Evaluation of the MHAAT Proof of Concept, conducted by NSW Ambulance Executive Director of Clinical Governance and Executive Director of Service Delivery
- October 2015 – Memorandum of Understanding 'business as usual' signed by WSLHD Chief Executive Danny O’Connor and NSW Ambulance Commissioner David Dutton
Implementation sites
Cumberland Hospital, WSLHD
Partnerships
- NSW Ambulance
- NSW Police
Results
The MHAAT model has shown to significantly improve the quality of care provided to mental health consumers, while saving costs and maximising use of other mental health resources. Within three months of implementation, MHAAT diverted 76 per cent of calls away from Cumberland Hospital ED, 24 per cent of which were provided with referrals to mental health services in the community. As a result, there is less unnecessary ED presentations and multiple transfers of care.
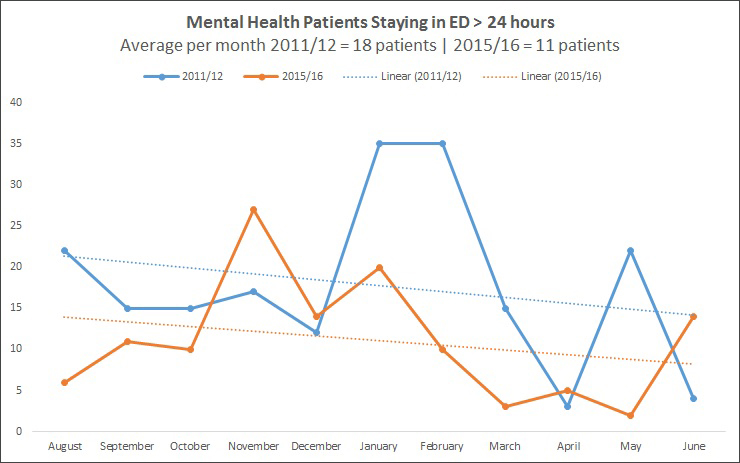
In 2016, 816 consumers were assessed by the MHAAT. Of these, 37.5 per cent were admitted to a mental health unit, 38 per cent were reviewed in Cumberland Hospital ED and 24.5 per cent were managed in the community. MHAAT also reduced the number of mental health consumers staying in the ED more than 24 hours, from 18 patients in 2011-12 to 11 in 2015-16 (Figure 1). Trends show this average will continue to decline, which means consumers are receiving appropriate care in a timely manner.
The pairing of a paramedic and mental health clinical nurse consultant resulted in better teamwork and partnership, with surveys showing that each clinician learned from the other while developing valuable skills for their own role. In November 2015, a Memorandum of Understanding was signed between WSLHD and NSW Ambulance to continue the service. It is now a service delivery model for Community Health and Outpatient Care, with data collected and evaluated for activity based funding purposes.
Awards
- 2014 Council of Ambulance Authorities Award - Clinical Capability
- 2017 NSW Health Awards Winner - Excellence in the Provision of Mental Health | View a poster from the 2017 NSW Health Awards
Lessons learnt
MHAAT had limited publicity when it was launched and few people knew about it, even within WSLHD and local emergency services. A collective understanding of the MHAAT service within mental health facilities, NSW police and community mental health services is important.
Access to electronic medical records is valuable when performing mental health assessments in outpatient settings, to check patient mental health history, document mental health triage and add progress notes. It is also a tool to enter data for activity-based funding purposes.
The team faced resistance to change when implementing the project. This was addressed by communicating with staff and doctors and distributing a memorandum from the director of nursing about the change. To ensure best possible care to mental health patients, collaboration with NSW Ambulance and clinical staff was key.
The model of care is more effective when local community mental health teams are involved. This not only maximises the efficiency of resources, but provides consumers with faster follow-up and better access to community-based mental health treatments.
If Activity-Based Funding is included within the model of service delivery, there needs to be a thorough understanding of the model by clinicians, to ensure they document the events occurring during service delivery accurately.
Further reading
- NSW Ambulance. Mental Health Acute Assessment Team Proof of Concept: Fact Sheet.
- Faddy SC, McLaughlin KJ, Cox PT e al. The Mental Health Acute Assessment Team: a collaborative approach to treating mental health patients in the community. Australasian Psychiatry 2017;25(3):262-65.
Contact
Junn Miranda
Acting Clinical Nurse Consultant, Mental Health Acute Assessment Team
Mental Health Services
Western Sydney Local Health District
0422 328 506
junn.miranda@health.nsw.gov.au
Anita Das
Acting Clinical Nurse Consultant, Mental Health Acute Assessment Team
Mental Health Services
Western Sydney Local Health District
Phone: 0409 487 293
Anita.Das@health.nsw.gov.au