This project conducted a review of the care delivered to patients admitted to the oncology and palliative care wards at Westmead Hospital. As a result, changes were implemented that aimed to improve the coordination of care, reduce length of stay and streamline the discharge process.
View a poster from the Centre for Healthcare Redesign graduation, August 2017.
Aim
To ensure oncology inpatients at Westmead Hospital are provided with timely access to appropriate, high-quality care and an optimal patient experience, by:
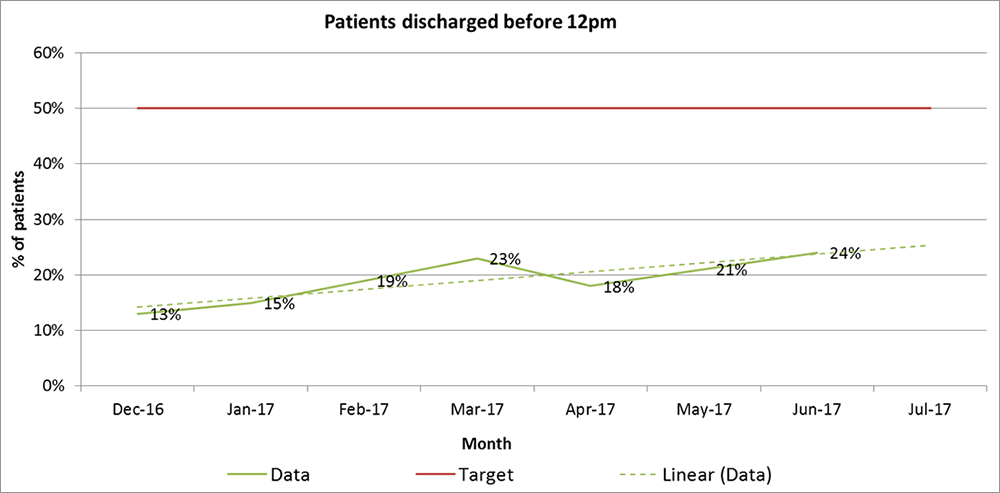
- increasing the proportion of patients discharged prior to midday from 18% to 50% by August 2017
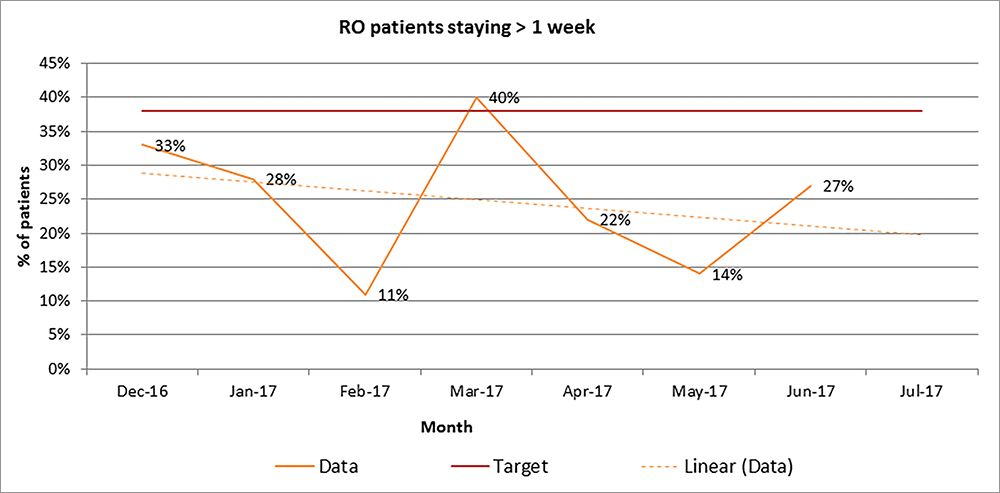
- reducing the proportion of radiation oncology inpatients staying more than one week from 48% to 38% by August 2017.
Benefits
- Improves the patient experience and quality of inpatient care.
- Provides timely access to inpatient cancer services.
- Strengthens communication and relationships between allied health, medical and nursing teams.
- Enhances the presence of radiation oncology staff on inpatient wards.
- Improves the knowledge and skills of rotating medical staff.
- Streamlines discharge planning and reduces delays.
- Reduces average length of stay for radiation oncology, medical oncology and palliative care patients.
Background
The inpatient cancer service at Westmead Hospital is a core part of the Western Sydney Cancer Network. Inpatient care offers a broad range of essential services, including radiation therapy and chemotherapy delivery, management of acute and late toxicity of cancer treatments, symptom control, palliative care, psychosocial and allied health support. This is achieved through a multidisciplinary team approach across all services.
There are over 1000 cancer inpatient admissions to Westmead Hospital each year, with only around 120 of these admissions via a radiation oncologist. An audit conducted in 2016 showed that the length of stay for radiation and medical oncology inpatients had increased by more than two days compared with the same period the previous year. An increased length of stay can lead to a higher risk of infection, morbidity and mortality. It can also negatively impact access to inpatient services and bed availability, cancer patients’ experience of inpatient care, staff workload and resource capacity.
Prior to the project, there was a growing consensus among cancer care staff across all levels and specialities that inpatient care ‘could be done better’. Anecdotally, staff reported a number of challenges and frustrations regarding inpatient patterns of care. These included:
- limited and unpredictable presence of radiation oncology medical staff in the inpatient ward
- poor communication between allied health staff and medical teams, resulting in a high rate of inappropriate referrals
- significant delays during the discharge process and on the day of discharge, which negatively impacted the patient experience.
Implementation
The following solutions were implemented between February and June 2017.
1. Electronic patient journey board meeting
Electronic patient journey board meetings are held at 9am from Monday to Friday. These meetings are designed to help staff plan ahead and manage patient flow. However, prior to the project they functioned more as a medical handover. Meetings took longer than the allocated 30 minutes and there was minimal input from allied health services. An opportunity was identified to enhance the functionality of this meeting and improve communication between teams.
A set agenda with seven discharge-specific questions was developed in small focus groups of medical, nursing and allied health representatives. The questions were asked 48 hours in advance of the patient’s estimated discharge date. The solution was implemented in two phases: phase one to improve the operational function of the journey board and phase two to improve content delivery. The agenda helped refocus the attention on the patient journey and streamline discharge planning.
2. Radiation oncology advance trainee
A radiation oncology advance trainee was allocated to the oncology inpatient ward, with the aim of managing patient care. The position was designed to act as a single point of contact for inpatient ward consults and represent radiation oncology at inpatient multidisciplinary meetings and daily reviews. They were responsible for facilitating bookings, planning and expediting all inpatient radiotherapy. This position was filled using the existing advance trainee workforce and workloads were readjusted to suit the new responsibilities. The advanced trainee helped promote timely discharges and reduce length of stay for radiation oncology patients.
3. Ward orientation session
A ward orientation session for clinical staff was introduced at the beginning of each medical term, to explain the role of and services provided by allied health teams, pharmacy, nursing and clinical documentation specialists. Previously, there was no formal orientation for new staff about the team and ward processes.
This solution was developed in collaboration with the ward team and comprised a 30-minute orientation session delivered to interns, residents and registrars on the second day of term. It allowed the ward team to formally introduce themselves and discuss planning processes and best practice methods of communication. The session has helped medical staff transition into their new placement and increased interactions between medical and allied health services.
Project status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Key dates
May 2016 – August 2017
Implementation site
Westmead Hospital, Western Sydney Local Health District
Partnership
Centre for Healthcare Redesign
Evaluation
A full evaluation will measure the following key performance indicators:
- percentage of patients discharged before 12pm
- average length of stay for radiation oncology, medical oncology and palliative care patients
- 28-day readmission rates for radiation oncology, medical oncology and palliative care patients
- patient and staff satisfaction ratings
- number of ward orientations undertaken per year.
Monthly audits conducted between December 2016 and June 2017 found the percentage of patients discharged before midday was trending upwards, from 13% to 24% as shown in Figure 1. As of June 2017, the target of 50% had not been achieved. However, this may be due to the relocation and closure of the ward in December 2016. During this period, inpatient numbers were reduced by 40% and the remaining inpatient beds split over two locations. This made it difficult to measure the impact of solutions implemented.
Monthly audits conducted between December 2016 and June 2017 showed that the percentage of radiation oncology patients staying longer than one week was trending downwards, from 33% to 14% as shown in Figure 2. The project exceeded its target of 38% as a result of the solutions implemented.
Monthly audits of patient satisfaction conducted between January and June 2017 suggested the solutions did not have a negative impact on patient satisfaction.
Lessons learnt
- It’s important to maintain continuous engagement and communication with key stakeholders throughout the project.
- A clear clinical lead and active sponsor support is integral to the success of the project.
- Defining and maintaining the scope of the project can be challenging but is necessary for solutions to be effective.
Contact
Elizabeth Phillips
Innovation & Redesign Project Lead
Western Sydney Local Health District
Phone: 02 8838 6453
Elizabeth.Phillips1@health.nsw.gov.au
Dr Lucinda Morris
Radiation Oncologist
Western Sydney Local Health District
Phone: 02 9845 5200
Lucinda.Morris@health.nsw.gov.au