The Improving Medication Administration in Custody project improves the medication administration process for people in custody in NSW public correctional facilities.
View a poster from the Centre for Healthcare Redesign graduation November 2022.
Aim
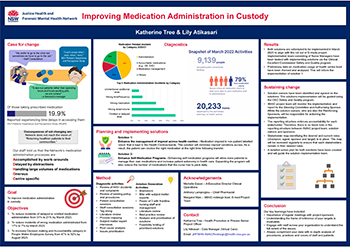
The goal of the project is to improve medication administration for people in custody across NSW adult settings by August 2023.
This will be measured by:
- Reduction in incidents of delayed or omitted medication administration from 31% to 21% by March 2023
- Reduction in incidents of wrong medication administrated from 17% to 7% by March 2023
- Increase in Justice Health NSW’s decision-making and accountability category in the People Matter Employees Survey from 47% to 52% by August 2023.
Benefits
Patients
- Patients receive the correct medication on time
- More patients will have full ownership and autonomy of their medication regimes
- Patients will improve their medication literacy
Staff
- Nurses manually pack and label less medications per day
- Nurses have more time to attend to primary health needs of patients
- Managers spend less time responding to incidents
- Clinicians have clear expectations of imprest medication
Healthcare system
- Reduced costs of reconciliation of medication-related incidents
- Reduced costs of time for staff to follow-up on medication administration delays and errors
- Reduced cost of express delivery of medication
Background
Each year, Justice Health NSW staff care for more than 30,000 patients, providing 800,000 occasions of service to people in courts, police cells, youth justice centres, correctional centres, inpatient settings, and in the community. Medication administration is vital to the health of the custodial population, yet the process is complex for both clinician and patient.
Diagnostic data indicates multiple safety concerns in the way medication is managed in the Justice Health NSW.
- 30 of 117 of patient complaints and 139 of 958 incidents reported during quarter 1 of 2021 calendar year are related to medication, making it the second highest reported incident category.
- 5 of 44 coronial recommendations as of the end of quarter 1 2021 calendar are related to medication processes and management.
- Medication related incidents account for the second highest incidents in 2020/21.
- Justice Health NSW currently has eighteen medication guidelines, protocols and procedures to guide the workforce and ensure safe medication management and practices. These multiple and diverse approaches to medication management create challenges for clinicians in keeping up with their responsibilities.
- Justice Health NSW is currently using a paper-based medication process (prescribing and faxing of medication charts between locations).
In NSW public prisons, nurses pack and administer medications daily for the majority of people in custody. Nurses check over 7,000 medication charts daily to prepare for medication administration. That is equivalent to four out of every five persons in custody. A health centre pack 50 to 150 medication bags everyday. A flow on effect is that nurses spend between one to four hours packing medication daily.
During patient consultation, patients told us that they are most concerned when their medication is delayed or omitted. Delayed and omitted doses account for the highest percentage of medication administration incidents.
During staff consultation, clinician told us that medication administration involves significant manual work and there are many workarounds created with the aim to create safer practices for staff and patients.
All of the above demonstrates the complex challenges of medication administration and the needs for solutions to ensure safety for staff and quality and continuity of care for patients.
Implementation
Solution 1: Enhance the management of imprest across health centres
Medication imprest is non-patient labelled stock that is kept in the health centres or wards. This solution will minimise imprest variations across facilities as each health centre will adopt one of the available standardised imprest lists. Viewing other health centres imprest list will provide nurses better visibility in identifying medications that are not routinely available at the receiving health centre. As a result patient can receive the right medication at the right time following transfer.
Solution 2: Enhance self-medication programs
Enhancing self-medication programs will allow more patients to manage their own medications and increase patient autonomy in healthcare. Expanding the program will also reduce the number of medications that a nurse has to pack daily. This will lead to fewer incidents related to medication administration.
Implementation measures
The number of patients on self-medication programs is increased
Streamlined business rules and processes for self-medication programs
Self-medication champion identified and every health centre
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- Start date: September 2022
- End date: August 2023
Implementation sites
All Justice Health NSW outpatient areas
Partnerships
- Centre for Healthcare Redesign
- Corrective Services NSW
Evaluation
Solution 1: Enhance the management of imprest across health centres
- Standardised imprest lists created for adult male, adult female and adolescent patients.
- 100% of health centres adopt one of the available standardised imprests
Solution 2: Enhance self-medication programs
- The number of patients on self-medication programs is increased by 10%
- Streamlined business rules and processes for self-medication programs
- Self-medication champion identified and every health centre
Lessons learnt
- Importance of regular meetings with project sponsors. This needs to be booked in advance.
- Understanding the frame of reference of your targets is invaluable.
- Engage with staff and patient across your organisation to understand the full extent of the issues.
- Always complement your data with in-depth analysis of procedures, actual practices, best practices and voices of staff and patients.
Further reading
Justice Health and Forensic Mental Health Network
Contacts
Katherine Tree
Health Promotion in Prisons Senior Project Officer
Justice Health NSW
Katherine.tree@health.nsw.gov.au
Lily Atikasari
Data Manager – Virtual Care
Justice Health NSW
Lily.atikasari@health.nsw.gov.au