The project focused on achieving better outcomes, reduced length of stay and improved experiences for patients admitted to Graythwaite Rehabilitation Centre (GRC), Ryde Hospital.
Aim
To improve the effectiveness and efficiency of the service provided to inpatients at GRC, by achieving the following objectives.
- 5% increase in patient experience from 80% to 85% by August 2020.
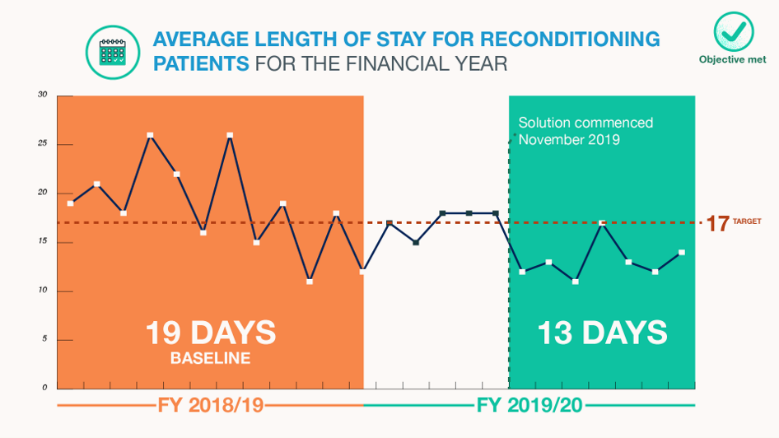
- 11% reduction in average length of stay for Reconditioning patients from 19 days to 17 days by August 2020.
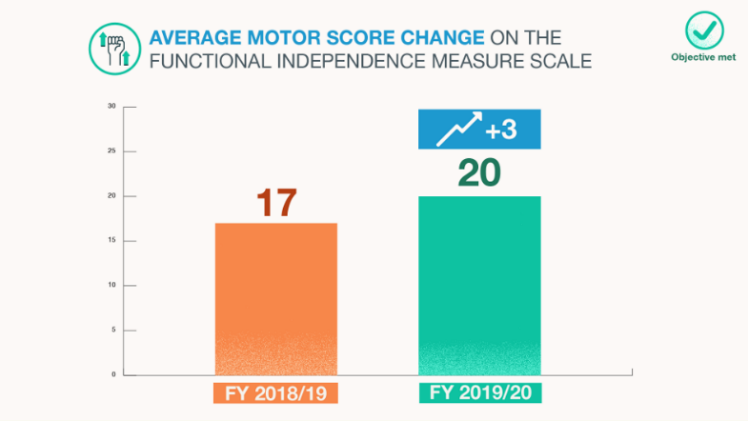
- Improve functional outcomes by an 11% increase in average Functional Independence Measure (FIM) motor score change for GRC patients from 17 to 19 points.
Benefits
For patients
- Improved communication of the expectations of rehabilitation to patients, through provision of an innovative approach that is engaging and relevant.
- Reduction of the mismatch between patient and carer and staff expectations.
- Improved experience at GRC.
- Timely referrals and early identification of barriers to meeting patients’ goals and discharge plans.
- Improved quality of life with earlier resumption of normal living.
For staff
- Standardised processes.
- Increased awareness of rehabilitation outcomes and benchmarks.
- Improved accuracy in data reporting.
- Increased staff satisfaction from improved collaboration and early involvement in project activities.
For the healthcare system
- Reduced wait times for admission to GRC and improving patient flow from acute care to rehabilitation.
- A more cost-efficient service, demonstrated by improved functional gains to length of stay.
- Increased GRC’s credibility as a rehabilitation provider.
Background
Rehabilitation is a vital aspect in the recovery process after illness or injury. It aims to minimise and/or prevent disability, improve health outcomes, reduce disease burden, reduce costs of social services, improve one’s participation in life, and improve quality of life.1
A service review in 2019 highlighted that patients admitted to GRC for rehabilitation were staying longer, and functional outcomes were less than those in comparable services within Northern Sydney Health District. In the financial year 2018-19, patients classified for rehabilitation due to reconditioning following illness made up the largest population seen in GRC (41%). This group of patients had longer average length of stay by three days compared to a district peer hospital, and also longer than national benchmark targets. Unfortunately, in the financial year 2018-19, GRC patients made lower functional improvements by scoring two points less (FIM average motor score change) than other district rehabilitation services.
Delaying the patients’ resumption to normal living in the community and at a poorer functional level, will reduce quality of life. Staying in hospital longer also runs the risk of acquiring healthcare associated infections, furthering a longer recovery time, illness and longer stay.2-3
Not only will this increase cost to the hospital, longer length of stays in rehabilitation will have an impact on patient flow within the healthcare system. A decreased bed availability will lead to unnecessary bed occupancy days in acute care.4
Implementation
Focus areas
Three key focus areas were identified to have greatest impact on GRC outcomes.
- Communication to patients and carers regarding rehabilitation expectations and the rehabilitation journey.
A patient experience survey conducted in May 2019 highlighted opportunities for improvement, especially in providing information to patients and carers regarding setting expectations. From interviews, 64% of patients felt they had limited understanding of rehabilitation.
- Multidisciplinary team communication and processes to support discharge planning.
Staff had expressed that the disorganisation and variation in rehabilitation processes were reflected in frequent delays in discharges. 38% of patients had to have their stay extended from the initial estimated discharge date given.
- Functional gains data reporting
Diagnostic activities revealed poor and inconsistent data quality. On a mandatory reporting form that details the functional gains of patients and their classification reason for undergoing rehabilitation, 53% of the information was incomplete or inaccurate.
Solutions
Four high impact solutions were identified to address the three focus areas and consequently, the project objectives.
Solution 1: Using the AROC AN-SNAP calculator to formulate an estimated discharge date
Australasian Rehabilitation Outcomes Centre (AROC) is the national rehabilitation medicine clinical registry of Australia and New Zealand. This solution uses a tool created by the registry that assist in formulating a patient’s estimated discharge date, based on expected functional change and length of stay outcomes in line with national benchmark targets.5 Facilitating this solution required redefining the processes to ensure a role-dependent nature, with timely and accurate coding of patient information. Accurate coding and reporting will demonstrate fidelity in GRC’s reporting of functional outcomes.
Solution 2: Patient-centred welcome film
This solution was generated by staff, highlighted as high impact on improving the patients’ experience by innovatively communicating rehabilitation expectations. The high cost of filming required seeking funding opportunities. The working party was successful in acquiring an innovation grant to fund the completion of a patient centred orientation film. The film is due for production in October 2020, with roll out in use by end of 2020. Outcome and process measures will encompass the patient-reported experience measure, solution-specific surveys and interviews.
Solution 3: GRC discharge decision-support tool
A decision-support tool was created to support the multidisciplinary team in determining a patient’s discharge readiness, and ensure consistency in discharge decision making. This was generated from staff workshops and refined with the support from literature.6 The tool has been piloted, refined and now implemented in all case conferences. Monitoring the length of stay and number of patients meeting their initial estimated discharge date is ongoing.
Solution 4: GRC orientation and education program
A GRC orientation resource was created to meet the needs of staff starting work at GRC. This solution was generated from staff workshops and further refined with a staff survey. This is now available for use with a regular review date to ensure relevance of information.
Development of a GRC team education program was developed by a working party and feedback from staff surveys. The program aims to improve GRC cohesion as a team, improve communication between staff, patients and carers, and increase awareness of rehabilitation outcomes. This solution was delayed in its launch due to the COVID-19 pandemic but has now started through teleconferencing, with the incorporation of case studies to aid reflection and learning with onward implementation of actions.
Change
All four solutions were staff generated, with patient and consumer feedback to support the change idea.
Early collaboration with GRC staff and involvement in project activities, coupled with strong sponsorship were key factors in achieving change.
Working parties was created from champions identified for each solution. Members of the working party were involved in solution communication, solution development and data capturing.
The project team are now working to support the solutions through to sustainability and establish solutions as business as usual.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- July 2019 - Project start
- August 2019 - Diagnostic phase
- October 2019 - Solution development and testing
- Feb 2020 - Implementation of solutions
- March 2020 - COVID-19 pandemic delayed implementation
- June 2020 - Recommenced implementation
- Sept 2020
- Evaluation in progress and progression to sustainability
- Ongoing development of patient-centered welcome film
- December 2020
- Evaluation completion of implemented solutions
- Roll-out of patient-centered welcome film
Implementation sites
Graythwaite Rehabilitation Centre, Ryde Hospital. Northern Sydney Local Health District.
Partnerships
Centre for Healthcare Redesign
Results
Solution 1: Using the AROC AN-SNAP calculator to formulate an estimated discharge date for Reconditioning patients, and Solution 3: GRC discharge decision-support tool for all rehabilitation patients
Monitoring the number of patients achieving their initial estimated discharge date showed an average of 57% patients meeting their init l estimated discharge date for 2020 to date.
Quick win: Having a second computer at journey board meetings for referrals.
A spot audit of one week showed that 16 referrals were required. A second computer was present only 20% of the time, however 15 referrals were completed within an hour of the meeting. This is a win for early referrals and early discharge planning.

Solution 2: Patient-centred welcome film
This has yet to be evaluated as the solution is still in development. A repeat of the patient- reported experience measure, the Australian Modified Client-Centred Rehabilitation Questionnaire will be the primary measure. By addressing rehabilitation expectations, highlighted as the major concern from patients from our service, it is hypothesised that this solution will have the highest impact on patient-experience. Evaluation will also include patient interviews and evaluation will start as soon as the solution is rolled out.
Solution 4: GRC orientation and education program
Repeat of a solution-specific staff survey and the patient reported-experience measure will be used for evaluation three months post-implementation. This solution is hypothesised to benefit communication with patients and carers, subsequently improving the coordination of discharge planning and patient’s understanding of rehabilitation.
Objectives
11% reduction in average length of stay for Reconditioning patients from 19 days to 17 days by August 2020.
This objective was achieved. For the financial year 2019-20, there was a 21% reduction to 15 days. Post- implementation of solutions showed a reduction to 13 days that remained below the target of 17 days.
Improve functional outcomes by an 11% increase in Functional Independence Measure motor score change for GRC patients from 17 to 19 points.
This objective was achieved with an 18% improvement.
5% increase in patient experience on the patient-reported experience measure from 80% to 85% by August 2020.
This objective, measured using the Australian Modified Client-Centred Rehabilitation Questionnaire gave a score of 91%, showing a 14% improvement.
Interpretation
The results need to be interpreted with caution due to the impacts of COVID-19. Please see Lessons learnt.
Lessons learnt
A major impact on project implementation was the COVID-19 pandemic. As a result, the rehabilitation service within the health district was required to adjust capacity to meet the needs of COVID-19 contingency plans. GRC reduced its number of beds by half due to a reduction in demand for rehabilitation. This resulted in a reduced volume of inpatients admitted to GRC. Demand for inpatient rehabilitation also reduced as elective surgery ceased. All patients were admitted to one ward which created both challenges and opportunities.
Operating as one ward enabled rehabilitation processes to be consistent and improved ease in implementing change. Staff have proved themselves to be flexible and resilient.
- The project team have gained skills and knowledge with a greater confidence to ‘trust the process’ by the Centre for Healthcare Redesign methodology.
- Strong sponsorship is vital to achieving project success.
- Changing culture is a challenge, and sub-cultures can be revealed as solutions are moved towards implementation and sustainability.
- Engaging staff early in the process helped to identify champions and agents for change.
- Power of the patient story to aid all communications and was powerful in engaging all staff groups in the change.
- Be flexible and adaptable – completing a project during Christmas holiday period and having COVID-19 highlighted the importance of timing and momentum.
- Undertaking a Redesign project has led to other opportunities for the team including a successful Innovation Award grant, with opportunities to network and to communicate to a wider audience.
References
- Agency for Clinical Innovation. Principles to support rehabilitation care [Internet]. Sydney: Agency for Clinical Innovation; 2019 [cited 2019 Oct 28]. 24p.
- Australian Commission on Safety and Quality in Health Care. Healthcare-Associated Infections [Internet]. Sydney: Australian Commission on Safety and Quality in Health Care; 2018 [cited 2019 Nov 1]. 35p.
- Better Health Channel. Preventing healthcare associated infection (HAI) [Internet]. Victoria: Department of Health and Human Services, State Government of Victoria, Australia; 2015 Jul 31 [cited 2019 Nov 1].
- New PW, Jolley DJ, Cameron PA, Olver JH, Stoelwinder JU. A prospective multicentre study of barriers to discharge from inpatient rehabilitation. Med J Aust [Internet]. 2013 Feb [cited 2019 Sep 27]; 198 (2), 104-108. DOI: 10.5694/mja12.10340.
- University of Wollongong Australia. Australasian Rehabilitation Outcomes Centre [Internet]. Wollongong: University of Wollongong Australia; Date unknown [cited 2019 Oct 23].
- Burns AS, Yee J, Flett HM, Guy K, Cournoyea N. Impact of benchmarking and clinical decision making tools on rehabilitation length of stay following spinal cord injury. Spinal Cord [Internet]. 2013 Feb [cited 2019 Oct 15]; 51(2): 165-169.
Contact
Philippa Wilford
Acting Team Lead Occupational Therapist
Graythwaite Rehabilitation Centre
Ryde Hospital, Sydney
Phone: 02 9858 7149
philippa.wilford@health.nsw.gov.au
Sharon Fok
Senior Physiotherapist Rehabilitation
Graythwaite Rehabilitation Centre
Ryde Hospital, Sydney
Phone: 02 9858 7144
yoke.fok@health.nsw.gov.au
Esther Ng
Nurse Manager Performance and Access
Ryde Hospital, Sydney
Phone: 02 9858 7545
Esther.Ng@health.nsw.gov.au
Alanna Brown
Nurse Unit Manager
Graythwaite Rehabilitation Centre
Ryde Hospital, Sydney
Phone: 02 9858 7125
alanna.brown1@health.nsw.gov.au