This project creates efficiencies in the provision of non-acute mental health beds across the Northern Sydney Local Health District by improving referral and communication processes and providing a better overall experience for patients and staff.
View a poster from the Centre for Healthcare Redesign graduation, August 2018.
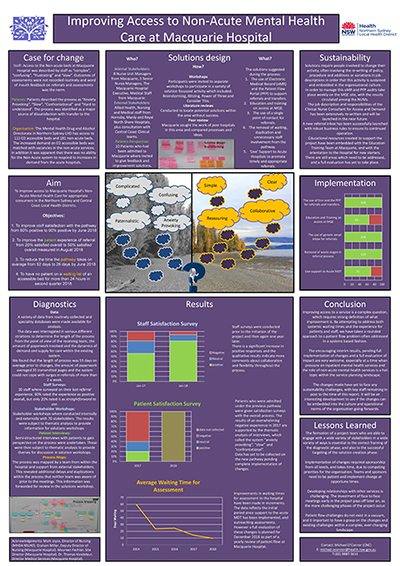
Aim
To reduce the wait time to transfer from an acute to a non-acute mental health bed in Northern Sydney Local Health District from 55 to 25 days within 12 months.
Benefits
- Improved patient satisfaction through reduced wait time for transfers between acute and non-acute care.
- A more transparent system of referral, assessment and transfer, to enable patients to understand their clinical path and participate in it.
- Reduced delay in transferring to an appropriate bed to reduce the overall length of stay for the patient.
- Staff members will experience a smoother and more responsive clinical pathway between acute and non-acute care.
- Staff members can articulate and understand the steps within the clinical pathway.
- The healthcare system will benefit from a more responsive system of transfer from acute mental health beds to non-acute mental health beds, which in turn eases the pressure on Emergency Department waiting times.
Background
Between 2014 and 2017, referrals to Macquarie Hospital increased by 338% and the number of patients assessed increased by 418%. This increase in demand led to greater scrutiny on the process of referral, assessment and admission, and stretched hospital resources. The process was slow, complex, and unresponsive to bed pressure in the acute sector. This meant delays in referrals, misinformation for patients, and a flow-on effect to the length of stay in acute mental health wards and ultimately emergency departments.
Addressing the clinical pathway to accessing non-acute mental health beds will lead to more timely access and reduced patient waiting time in acute wards. In turn, this will reduce the cost of treatment per capita and improve the overall patient and staff experience.
The NSW 2021 and the Living Well Strategic Mental Health plans aim 'to provide world-class clinical services with timely access and effective infrastructure'. Creating a more transparent and responsive system allows referring staff and patients to see how decisions about care are made and supports informed decision making and a greater sense of collaborative care.
In addition, timely access to non-acute services will promote recovery orientated practice by allowing delivery of specialised care at the correct point in the patient journey towards community living.
Implementation
Following the diagnostic stage, the project team came up with five key solutions.
1. Support the acute multidisciplinary team decision making process
Macquarie Hospital offers attendance or distance input to these meetings in order to assist with the decision to refer a patient. This solution is designed to reduce the number of inappropriate referrals and remove the wait to refer caused by a lack of information in the acute multidisciplinary team.
Results are evaluated by a repeat questionnaire given to acute staff to assess their ability to request support, and the quality of the support provided. In June 2017 60% of staff felt confident in their ability to make this decision within a multidisciplinary team.
2. Reduce duplication in referral stage
The clinical director and process owner have been commissioned to review the pathway with input from stakeholders with a focus on removing wasted time, duplication of information, inappropriate use of clinical staff to complete administrative tasks and appropriate delegation of assessments to more junior staff. This solution is designed to reduce the amount of time and information being duplicated in the referral stage of the clinical pathway.
3. Establish a single email inbox for all referrals to Macquarie Hospital
Designed to reduce confusion and issues when the clinical nurse consultant (CNC) for access and demand is on leave, or leaves the job. Previously, all referrals to Macquarie Hospital were emailed directly to the CNC. This led to confusion, lost referrals, and issues when the CNC was out of the office.
4. Increase use of the electronic medical record and Patient Flow Portal to improve information sharing on referrals
Designed to increase transparency of the system and reduce the clinical load on referring staff members. Referral progress was previously managed within an off-line database by the CNC for access and demand. This led to confusion and uncertainty for all staff when this person was unavailable. By migrating the information to the electronic medical record (documented outcome of referrals) and the Patient Flow Portal (patient and referring staff information documented and available) this issue has been completely mitigated.
5. An education and training package in patient flow in mental health
It was apparent from interviews with staff that nurse unit managers and senior nurse managers where unfamiliar with the Patient Flow Portal and changes to patient flow in mental health. An education package has been proposed and is currently in development. This will be delivered to all nurse unit managers and senior nurse managers by the end of 2018.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
30 August 2017 to 1 October 2018.
Implementation sites
- Macquarie Hospital
- Manly District Hospital East Wing
- Hornsby Ku-ring-gai Hospital Adult Mental Health Unit and Mental Health Intensive Care Unit
- Royal North Shore Hospital Adult Mental Health Unit
Partnerships
- Centre for Healthcare Redesign
- CHR representatives in Northern Sydney Local Health District
- Whole of Hospital Project Mental Health Branch
- Non-acute benchmarking team at INFORMH
Results
- Some changes to practice have already been initiated and completed. We expect all recommended solutions to be completed by 30 September 2018
- Since March 2018, 100% of assessments have had an outcome documented in the electronic medical record and 90% of accepted patients have been documented in the Patient Flow Portal. This allows patient flow managers and nurse unit managers to communicate and plan patient movement more effectively.
- In June 2017 the average referral size to Macquarie Hospital was 35 pages, 90% of which was duplicated from the electronic medical record. In June 2018 the average referral size was five pages, 40% of which was duplicated from the medical record.
- The increased use of IT systems and reduced paperwork for referring staff has been completed and evaluated positively with a reduction of 10 days on average to create a referral using the new system.
- Staff have been re-surveyed regarding their view of the referral pathway in general, with an increase in positive responses from 60% in 2017 to 90% in 2018.
- There has been a reduction in the time waiting for assessments from 24 days in 2016 to 14 days in 2018.
- Use of the bed state at Macquarie Hospital has increased from 91% (July 2016) to 94% (July 2018) which represents six more beds being used on average.
- Patient interviews where undertaken at the start of the project, but a follow up has yet to be conducted on the patient’s view of the clinical pathway.
Lessons learnt
- Engaging staff early in the process is really valuable for their continued support at implementation stage.
- The way people feel about things is just as important, if not more important than the story the numbers tell.
- Face to face communication is worth the investment of time.
- Implementing change will take a considerable amount of time and resources. The quicker it needs to be, the more resources it will take.
- The project team and sponsor need to meet regularly and be hopeful about change.
Contact
Michael O’Connor
Clinical Nurse Consultant (Clinical Access and Demand)
Macquarie Hospital
Northern Sydney Local Health District
Phone: 02 9887 5614
michael.oconnor@health.nsw.gov.au