Optimise clinical care and experience provided to colorectal patients undergoing bowel resection (with or without stoma) at RNSH through:
- Provision of an intensive preoperative education package to patients and carers/family
- Creating a standardised care pathway for the multidisciplinary team to follow throughout the patient’s journey, which incorporated principles of Enhanced Recovery After Surgery (ERAS) for Colorectal Surgery.
Aim
To improve colorectal patients’ experience and outcomes through optimising their journey at Royal North Shore Hospital (RNSH) by April 2020 through the following objectives.
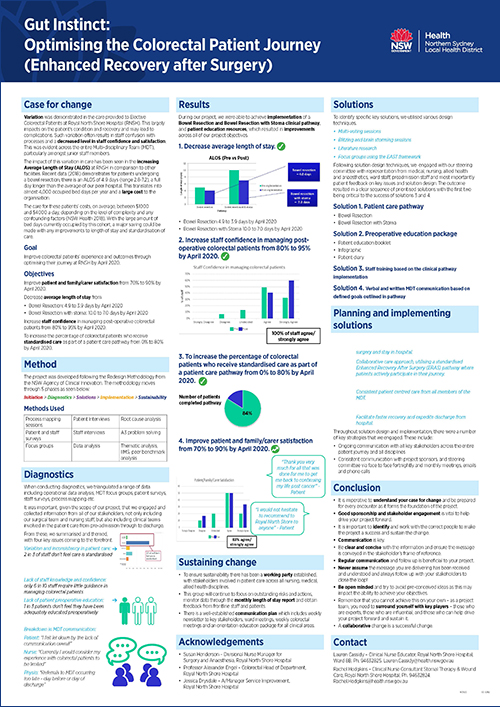
- Improve patient and family/carer satisfaction from 70% to 90% by April 2020.
- Decrease average length of stay from:
- bowel resection: 4.9 to 3.9 days by April 2020
- bowel resection with stoma formation: 10.0 to 7.0 days by April 2020.
- Increase staff confidence in managing post-operative colorectal patients from 80% to 95%.
- Increase the percentage of colorectal patients who receive standardised care as part of a patient care pathway from 0% to 80% by April 2020.
Benefits
Patient
- Greater ownership of their journey.
- Standardised care across all members of their team.
- Decrease readmission rates post discharge from hospital.
Organisational
- Higher patient flow through the department.
- Reduced wait times for surgical procedures and ability to meet surgical waitlist performance indicators.
- Improved value of care at RNSH.
Staff
- Increased staff satisfaction.
- Apply evidence-based care in the workplace.
- Improve understanding of department expectations.
- Increase staff confidence/competence/satisfaction caring for colorectal patients.
Program status
Program dates
The project was conducted from April 2019 – April 2020
- Inaugural steering committee meeting and establishment of governance 1 April 2019
- Prioritisation of key issues 30 May 2019.
- Solution generation and development completed by 23 August, including:
- development of two standardised care pathways (bowel resection with and without stoma formation)
- development of patient education resources (including infographic, education booklet and patient diary)
- Pilot commenced 11 November 2019
- Establishment of working party for sustainability
- Pilot completion 1 May 2020
- Evaluation phase start: 16 March 2020
- Evaluation phase end: 6 April 2020
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Background
The colorectal surgical patient commonly presents to hospital for surgical intervention for various conditions affecting the small and large bowel and can pose a large burden of disease on the individual and healthcare system.1,2 Surgical interventions can range from minor to major complexity, with care for patients beginning prior to admission, and continuing throughout their entire hospital stay. Therefore, care does not remain solely with the surgeon, but with various staff throughout the multidisciplinary team.
Variation was demonstrated in the care provided to these patients at RNSH, which can have large impacts on the patient’s condition and recovery and may lead to complications. Additionally, the variation often results in staff confusion with processes and a decreased level in staff confidence and satisfaction. This was evident across the entire multidisciplinary team, especially amongst junior staff members.
Furthermore, the impact of this variation in care has been seen in the increasing average length of stay at RNSH in comparison to other facilities. Recent data (2018) demonstrates for patients undergoing a bowel resection, there is an average length of stay of 4.9 days (range 2.8-7.2), a full day longer than the average of our peer hospital rates. This translates into almost 4,000 occupied bed days per year and a large cost to the organisation.
The care for these patients’ costs, on average, between $1000 and $4000 a day, depending on the level of complexity and any confounding factors (NSW Health 2018). With the large amount of bed days currently occupied by this cohort, a major saving could be made with any improvements to length of stay and standardisation of care.
Unwarranted clinical variation is a key priority and opportunity for improvement amongst this patient cohort, and for the facility of RNSH, and not only ensures optimal outcomes for our patients, but also to ensure that our staff are equipped with evidence-based care delivery.
Implementation
Initiation
Early establishment of sponsorship and governance, team members and ways of working was critical in the early phase of the project. Identification and communication with key stakeholders, including case for change and project objectives was also undertaken once the scope of the project was established. Continued communication and identification of risks and issues was essential to assist in mitigation.
Diagnostics
Understanding the problem presented was key to the diagnostics, including undertaking a range of diagnostic activities such as data analysis (audits, operational data, activity data etc.), process mapping sessions with our key stakeholders, focus groups and patient and staff surveys. Collating and triangulating the data to understand themes and key issues to present and prioritise with the steering committee to refine our scope with sponsor approval in preparation for our solutions phase.
Solutions
Development of solutions based on the diagnostics findings to align with our goal and objectives. This included; solution generation techniques such as literature review, site visits, brainstorming and blitzing sessions with key stakeholders. Identification of key solution leads during this time was also critical. Information was presented to our sponsors and Steering Committee so as to prioritise and sequence appropriately to ensure timeframes were met.
Frequent communication, tailored to each group of stakeholders was vital in achieving engagement throughout this phase. Small scale tests, pilots and frequent iterations also assisted in ensuring our solutions were fit for purpose prior to implementation.
Solutions which progressed to implementation included:
- Standardised pathways for bowel resection and bowel resection with stoma
- Education resources including education booklet, infographic and patient diary
Implementation
The Project Aim Strategy document outlined our implementation approach to the project. The implementation involved both operational and clinical leaders from the facility to ensure that it was planned, resourced and communicated via existing governance structures and communication channels. This was critical to ensure sustainability after the project team had ceased.
Education and communication to provide our stakeholders with the knowledge and confidence to complete the pathway, and implement the project across all departments and disciplines. It was also important to ensure that monitoring measures and a data plan were established, collected and reported regularly to objectively observe the progress being made, celebrating wins with the staff where appropriate and providing timely feedback to all. Specific data points included:
- percentage of patients successfully completing pathway
- length of stay
- staff experience
- patient experience.
Implementation sites
The project has been implemented at Royal North Shore Hospital. Whilst it included a small patient cohort, it was implemented across a number of clinical areas due to the nature of the pathway covering the entire patient journey.
Clinical areas
- Surgeons Private rooms
- Integrated Booking Unit, including the Nurse Screener
- Pre-Admission Clinic
- Short Surgical Stay Unit
- Operating Theatres and Recovery
- Ward 8B – Gastroenterology/Upper GI and Colorectal surgery
- Ward 8D – General Surgery
Stakeholders
- Medical stakeholders including colorectal surgeons, fellows, registrars and junior medical officers
- Anaesthetists (including Acute Pain Service Team)
- Nursing across specialty wards – nursing unit manager, clinical nurse educator, clinical nurse specialist, registered nurse, enrolled nurse, assistant in nursing
- Stomal therapy clinical nurse consultant
- Allied health staff – physiotherapist, dietician, occupational therapist, social worker, pharmacist
Partnerships
The organisations that we consulted with include:
- Agency for Clinical Innovation
- University of Tasmania
- Royal Prince Alfred Hospital
- Concord Repatriation General Hospital
- Westmead Hospital
Results
From implementing the project, we have been able to achieve a new patient journey. This now includes a clear, consistent and standardised approach to care from pre-admission to discharge.
The patients now receive an intensive pre-operative education package which provides them with information about their journey. Specifically, expected LOS, recovery, and their role during the entire admission. This has been proven to assist in a speedy recovery and be discharged as per the pathway.
Care is now provided following the ERAS pathway with the option for variance as per the surgeons and team discretion to ensure patients receive standardised care throughout their journey. Patients actively participate in their journey through using the patient recovery diary, which is also reinforced by the multidisciplinary team.
The new journey also provides consistent care from pre-admission clinic to discharge.
Results
- Implemented of both the pathways and the education resources, resulting in improvements across all of our project objectives.
- Our goals were achieved resulting in a 1 day length of stay improvement for bowel resection, and a 3 day length of stay improvement for those which also had a formation of stoma.
- We excelled in enhancing staff confidence in managing colorectal patients from 80% to 100%.
- Prior to commencing the project, we had 0% of elective colorectal patients on a standardised clinical pathway, such as ERAS. This patient cohort was receiving components of standardised care, however not physically placed on a pathway. Post the pilot, 84% of the patients received standardised care as part of a pathway.
- From all the patients who participated in the pilot, we consistently received positive feedback which was reflected in the both the quantitative and qualitative data. Currently, our data shows that 83% of patients/family and carers felt satisfied with the care that they received. Further to this, promisingly, the strongly agreed response that has improved since baseline.
- Overall, we have achieved our goal, which has resulted in a business as usual approach to ensure that ERAS is embedded across those clinical areas who have been actively involved with the project.
Lessons learnt
- It is imperative to understand your case for change and be prepared for every encounter as it forms the foundation of the project.
- Good sponsorship and stakeholder engagement is vital to help drive your project forward. It is important to identify and work with the correct people to make the project a success and sustain the change.
- Communication is key. Be clear and concise with the information and ensure the message is conveyed in the stakeholder’s frame of reference. Regular communication and follow up is beneficial to your project. Never assume the message you are delivering has been received and understood and always follow up with your stakeholders to close the loop!
- Be open minded and try to avoid pre-conceived ideas as this may impact the ability to achieve your objectives.
- Remember that you cannot achieve this on your own – as a project team, you need to surround yourself with key players – those who are experts, those who are influential, and those who can help drive your project forward and sustain it. A collaborative change is a successful change.
References
- Parkin CJ, Bell SW, Mirbagheri N. Colorectal cancer screening in Australia: An update. Australian Journal of General Practice. 2018;47( 12):859-863. Available from: https://www1.racgp.org.au/ajgp/2018/december/colorectal-cancer-screening-in-australia
- Comber H, Dwane F, Kelleher T, et al. Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions. National Centre for Biotechnology Information. 2012;12:7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3341181/
Further Reading
- Northern Sydney Local Health District. Strategic plan 2017-2022. Sydney: Northern Sydney Local Health District; 2018. viewed 15th April 2019. Available from: https://www.nslhd.health.nsw.gov.au/AboutUs/StrategicPlan/Documents/170711-FINAL-NSLHD_Strategic_Plan_A4_0407_LR.pdfn
- NSW Ministry of Health. AMB portal. [Database]. Viewed 16 April 2019.
- Dorrance, RH, MacKay JG, Molloy GR, O’Dwyer JP. Colorectal Surgery. Oxford, UK: Oxford University Press; 2010.
Contacts
Victoria Stockdale
Acting Divisional Manger of Surgery and Anaesthetics
Royal North Shore Hospital
Northern Sydney Local Health District
Phone: 02 9463 1923
Victoria.Stockdale@health.nsw.gov.au
Professor Alexander Engel
Colorectal Head of Department
Royal North Shore Hospital
Northern Sydney Local Health District
Phone: 0432 838 686
Alexander.Engel@health.nsw.gov.au
Elizabeth Bryan
Manager Service Improvement
Royal North Shore Hospital
Northern Sydney Local Health District
Phone: 02 9463 1908
elizabeth.bryan@health.nsw.gov.au
Lauren Cassidy
Clinical Nurse Educator (8B) and Project Lead
Northern Sydney Local Health District
Phone: 02 9463 2825
Lauren.Cassidy@health.nsw.gov.au
Rachel Hodgkins
Wound and Stomal Therapy Clinical Nurse Consultant
Royal North Shore Hospital
Northern Sydney Local Health District
Phone: 02 9463 2824
Rachel Hodgkins@health.nsw.gov.au