GPCanShare will implement a shared model of care that will include general practitioners in the multidisciplinary team across all areas of the colorectal cancer patient journey.
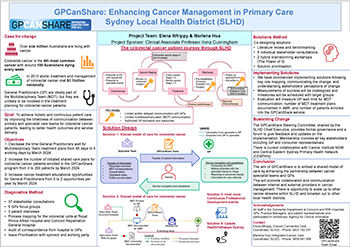
View a poster from the Centre for Healthcare Redesign graduation November 2022.
Aim
To achieve holistic and continuous care for colorectal cancer patients by:
- decreasing the time general practitioners wait for multidisciplinary team treatment plans, pre- and post-surgery, from 65 days to 5 working days by March 2024.
- increasing the number of initiated shared care plans for colorectal patients enrolled in the GPCanShare program from 0 to 200 patients by March 2024.
- increasing cancer treatment educational opportunities for general practitioners from 0 to 2 opportunities per year by March 2024.
Benefits
Patients
- Increased confidence in treating teams
- Increased information sharing between teams
- Less repetition of information
- More transparency about treatment plan
- More support in hospital and the community
- Better health outcomes and service delivery for colorectal cancer patients
Staff
- Increased confidence and use of virtual healthcare
- Redistribution of work
- Clarity of individual roles and responsibilities
- Increased education opportunities, resources, and knowledge sharing
- Increased general practitioner confidence in managing colorectal cancer in a primary care setting
Healthcare system
- Improved integration between hospital-based cancer care and primary care
- Alignment with the Sydney Local Health District Strategic Plan 2018-20231, by focusing on the development of integrated primary care in the community and shifting the balance of care and service into primary health.
- Alignment with the NSW Health Strategic Framework for Integrating Care2, by focusing on care coordination in a primary care setting and aiming to share information through rapid communication between teams and clinicians.
- Alignment with the Cancer Institute NSW Primary Health Cancer Framework3 and NSW Cancer Plan 2022-20274 by:
- understanding the importance of primary care in providing person-centred care to achieve better outcomes for people with cancer and improving integration
- communication between specialist and primary care so that accurate information is available to all providers to support them in making evidence-based decisions.
Background
Colorectal cancer is the fourth most common cancer with an estimation of a hundred Australians losing their lives to colorectal cancer every week.5, 6 Increased education and awareness, improved cancer screening, detection and treatment has seen a recent increase in cancer detection and subsequent survival rates.5 As the number of cancer survivors increase, increased pressure and workload is put on hospital-based specialist teams who follow up and monitor all existing patients as well as reviewing new patients.
There is scope for increased collaboration between primary and tertiary care. Currently, the role of primary care clinicians is important in the cancer patient journey for providing symptom management and holistic care.7,8 However, a comprehensive review of the role of primary care providers in cancer management, conducted in 2019 by Central Eastern Sydney Primary Health Network, found that a lack of communication between tertiary cancer teams and primary care practitioners resulted in difficulty in service navigation and limited support for patients with cancer and cancer-related palliative care needs.9
Currently, across the Sydney Local Health District, colorectal cancer treatment is specialist-based, meaning patients are being followed up by their cancer specialist teams and only see their general practitioners for non-cancer related comorbidities or for referrals. This model of care is costly and unsustainable as cancer survivors grow in number, requiring a shift to increase inclusion of primary care in the cancer patient journey.7,10 Shared care and integrated care models have been presented as the most responsive models of care to effectively meet the needs of patients and reduce financial
and workforce inefficiencies.7,8,10
Implementation
Project team
The project team is made up of an integrated cancer care coordinator and a cancer connected care coordinator. The GPCanShare Clinical Redesign Working Group provided insight and guidance on shaping the project until August 2022. The GPCanShare Steering Committee will oversee the implementation.
Key issues
Issues were identified through detailed process maps across the colorectal departments at Concord Repatriation General Hospital and Royal Prince Alfred Hospital. Individual stakeholder consultations were carried out to confirm each step of the process map, including patient surveys to understand the patients’ experience.
- Limited communication with general practitioners
- Limited multidisciplinary team communication
- No or limited general practitioner education and resources
- Lack of access to allied health services pre-surgery
Solutions
Workshops and a literature review were used to identify and prioritise solutions. It was noted at this point that, although a lack of access to allied health pre-surgery was important, it was out of scope for this clinical redesign project.
- Develop a shared care model for colorectal cancer patients
- Develop and implement a multidisciplinary team communication workflow for colorectal cancer patients
- Develop an information sharing protocol and update the multidisciplinary team terms of reference
- Increase continuous professional development events for general practitioners
- Review and update colorectal cancer links in HealthPathways Sydney
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Key dates
- 13 July 2021 – Project Initiation started
- 22 March 2022 – Diagnostics phase started (delayed start due to COVID-19)
- 28-29 March 2022 – Accelerated Implementation Methodology course
- 11 April 2022 – Establishment of GPCanShare Clinical Redesign Working Group
- 14 June 2022 – Solutions phase started
- 26 July 2022 – Implementation phase started
- 22 August 2022 – GPCanShare Clinical Redesign Working Group stopped
- 30 August 2022 – Sustainability workshops started
- 7 September 2022 – Establishment of GPCanShare Steering Committee
- 2023 – Evaluation phase to start
Implementation sites
- Colorectal Department, Royal Prince Alfred Hospital
- Colorectal Department, Concord Repatriation General Hospital
- General practices
- Central Eastern Sydney Primary Health Network
- Cancer Institute NSW
- Cancer Council NSW
- Centre for Healthcare Redesign, Agency for Clinical Innovation
- HealthPathways Sydney
- Chris O’Brien Lifehouse
Evaluation
A full evaluation will occur throughout 2023, noting each solution will be evaluated at different times.
- Specialist team and general practitioner surveys to monitor:
- satisfaction and feedback on use of multidisciplinary team forms
- satisfaction and feedback on modes of communication and timeliness.
- Patient, family and carers’ surveys to monitor satisfaction and feedback on GPCanShare as a service.
- Quantitative data collected on:
- number of patients discussed at the multidisciplinary team meetings and whether a multidisciplinary team template was used
- average time (compared to baseline) it takes for communication to be shared between the specialist teams and the general practitioners
- number of general practitioners that attend a continuous professional development event
- number of site visits for HealthPathways Sydney’s colorectal cancer links after site review and update (compared to baseline).
- A cost benefit analysis following transition of correspondence being sent from post to virtual methods.
Lessons learnt
- Everyone wants the same thing, you just need to break the wall between teams to get started
- Good sponsorship makes a world of difference
- There is always a work around
- Do not be afraid of radical ideas and shaking things up
- Trust the process and surrender to the Redesign methodology
- Leverage off existing platforms and capacity – make it work for you
- Understand your key stakeholder’s frame of reference
References
- Sydney Local Health District. Sydney Local Health District Strategic Plan 2018-2023. St Leonards, NSW: NSW Ministry of Health; 2018 [cited 20 Jun 2022].
- NSW Ministry of Health. NSW Health: Strategic Framework for Integrating Care. North Sydney, NSW: Ministry of Health; 2018 [cited 20 Jun 2022].
- Cancer Institute NSW. NSW Primary Health Care Cancer Framework. St Leonards, NSW: Cancer Institute NSW; 2020 [cited 20 Jun 2022].
- Cancer Institute NSW. NSW Cancer Plan 2022–2027. St Leonards, NSW: Cancer Institute NSW; 2022 [cited 20 Jun 2022].
- Australian Institute of Health and Welfare. Cancer in Australia 2021. Canberra, ACT: AIHW; 2021 [cited 20 Jun 2022].
- Bowel Cancer Australia. Bowel Cancer Facts. North Sydney, NSW: Bowel Cancer Australia; 2020 [cited 20 Jun 2022].
- Lisy K, Kent J, Piper A, Jefford M. Facilitators and barriers to shared primary and specialist cancer care: a systematic review. Support Care Cancer. 2021;29(1):85- 96. doi:10.1007/s00520-020-05624-5.
- Tran V-T, Barnes C, Montori VM, et al. Taxonomy of the burden of treatment: a multi-country web-based qualitative study of patients with chronic conditions. BMC Medicine. 2015 2015/05/14;13(1):115. DOI: 10.1186/s12916-015-0356-x
- Central Eastern Sydney Primary Health Network. Central and Eastern Sydney PHN 2019 Needs Assessment. Mascot, NSW: Central Eastern Sydney Primary Health Network; 2019 [cited 20 Jun 2022].
- Crawford-Williams FH, Haddock, R. Integrating shared care teams into cancer follow-up care models. Issues Brief 46. Canberra, ACT: Deeble Institute for Health Policy Research; 2022 [cited: 20 Jun 2022].
Further reading
- Royal Australian College of General Practitioners. Standards for general practices. East Melbourne, VIC: RACGP; 2020.
- Cancer Council Victoria and Department of Health Victoria. Optimal care pathway for people with colorectal cancer. Melbourne, VIC: Cancer Council Victoria; 2021.