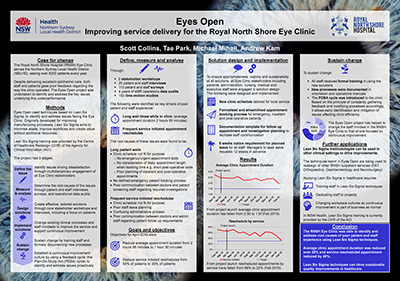
Eyes Open - Improving service delivery for the RNSH ophthalmology service
Summary
The ophthalmology service delivers excellent ophthalmic care, however, patient and staff feedback demonstrate that the service delivers a poor patient and staff experience. This project focused on identifying opportunities for improvement that relate specifically to patient and staff experiences, and then implementing sustainable changes to address these experiences.
View a poster from the Centre for Healthcare Redesign graduation, May 2019.
Aim
By 30 June 2019, to improve the patient experience in the following ways:
- reducing average clinic appointment duration from 2 hours 56 minutes to 1.5 hours
- reducing the ‘Did Not Attend’ rate from 8.5% to 5%
- reducing clinic reschedules from 12.4% to 8% and service initiated reschedules from 54.3% to 30%.
Benefits
- Improved patient experience as a result of decreased wait times and less crowded waiting rooms, as measured via patient satisfaction surveys and patient stories
- Increased efficiency of scheduling for new patients, leading to a reduction of the initial appointment waitlist
- Improved ophthalmology service access to the local Indigenous community as a result of established relationships with the respective local health districts’ Aboriginal Health Service
reduced costs and more efficient clinics due to a reduction in the Did Not Attend rate - Improved patient satisfaction
- Improved staff satisfaction
- Potential for achievements of the project to be rolled out to other ambulatory care clinics at Royal North Shore Hospital.
Background
Royal North Shore (RNS) Eye Clinic, based in the Ambulatory Care Centre, runs nine half-day registrar and consultant led clinics from 8am to 4:30pm each week. This clinic provides excellent ophthalmic care, however, feedback has demonstrated poor consumer experience due to the long wait times on the day of appointment. These clinics run 52 weeks of the year with reduced capacity for a four week period over the Christmas and January new year period.
Clinics are serviced by two registered nurses, an ophthalmology specialist nurse and an orthoptist. One senior and two junior registrars also cover the eye clinics, in addition to the emergency department and operating theatre lists. Half the clinics have a consultant present. There is no annual, sick, study or conference leave relief/cover for registrars or consultants. This often results in only one registrar being available to cover clinics, severely impacting on their ability to care for all patients on time.
As the only eye clinic in Northern Sydney Local Health District (NSLHD), the volume of patients referred to this service is extremely large. Recent data (2013 - 2017) demonstrates an increase in patient referrals via a number of pathways including; general practitioner and optometrist referrals, inpatient referrals (average of 2.4 patients per day) and emergency patient consults (average of 2.8 patients per day). Approximately 20% of all referrals received are for patients living outside of the NSLHD catchment (data from 2015 to 2016).
At the start of this project it was identified that, due to volume and a number of other factors, patients spent on average approximately three hours in clinic each visit, 45 minutes of which was required for their care. Appointment re-scheduling was also identified as an issue impacting upon patient experience, with over 12% of all appointments being rescheduled, mainly at the services request, not the patients and often due to poor leave planning.
Implementation
Project initiation included these steps.
- Established a sponsorship and steering committee (including two consumer representatives) to ensure agreement on scope, monitor progress against objectives and express, model and reinforce change to direct reports.
- Developed a stakeholder map and engagement plan to gain staff buy in and ownership across different organisational levels.
The project was formally launched with stakeholders, facility and local health district executive as a means to communicate and engage with all stakeholders.
A review of current practices was undertaken during the diagnostic phase, analysing over four years of data, surveying 99 consumers and engaging over 50 staff (including administration, nursing, medical and managerial staff). This identified a number of service related issues, which were directly related to specific roots causes that were addressed during the solution development phase.
Solutions included:
- a revised clinic schedule and on call appointment booking processes
- revised clinic documentation regarding patient consults, including follow up and discharge planning
- the development of fact and information sheets provided to patients in clinic and throughout the service journey. For example, at the time of surgery booking and post operatively
- a discharge and re-entry criteria to support registrar clinical decision making
- leave planning processes including a clinic modification plan for periods where medical staff are on leave.
Implementation included:
- formation of an implementation team consisting of local operational and clinical leaders to ensure implementation was planned, resourced and communicated via existing organisational channels to ensure that they were sustainable
- maintained staff engagement through branded and consistently structured written communication and monthly staff briefings
- establishment of consistent reporting tools and made results visible.
Status
Sustained - The project has been implemented, is sustained in standard business.
Dates
April 2018 – June 2019
Implementation sites
The project was implemented in the Ophthalmology Clinic at Royal North Shore Hospital, Northern Sydney Local Health District.
Partnerships
Agency for Clinical Innovation through the Centre for Healthcare Redesign
Evaluation
Objectives set for this project were ambitious, potentially too much so. On reflection our time in clinic objective exceeds performance of private practice settings that do not need to balance emergency department and inpatient demand. Project objectives and actual service performance are as follows.
- June 2019 goal: reducing average clinic appointment duration from 2 hours 56 minutes to 1.5 hours
August 2019 result: average clinic appointment duration is 1 hour and 58 minutes - June 2019 goal: reduce the ‘Did Not Attend’ rate from 8.5% to 5%
August 2019 result: the ‘Did Not Attend’ rate was reduced to 5.5% - June 2019 goal: reduce clinic reschedules from 12.4% to 8% and service initiated reschedules from 54.3% to 30%
August 2019 result: 37% of reschedules were at the service’s request
Lessons learnt
- Sponsorship and stakeholder engagement is the key. Identify who the right people are to make the project a success and what their drivers are. By communicating using their frame of reference their level of interest and buy in is immediately increased.
- Don’t be scared to make mistakes. Try things. Encourage staff around the project to try things. Nurture the sense that change is in the air by encourage all stakeholders to possess the power to make change happen.
- Find your data people and get to know them. Buy them lunch! Become their friend.
Contact
Scott Collins
Project Manager, Strategy and Service Integration
Royal North Shore Hospital
Northern Sydney Local Health District
02 94629863
Scott.collins@health.nsw.gov.au