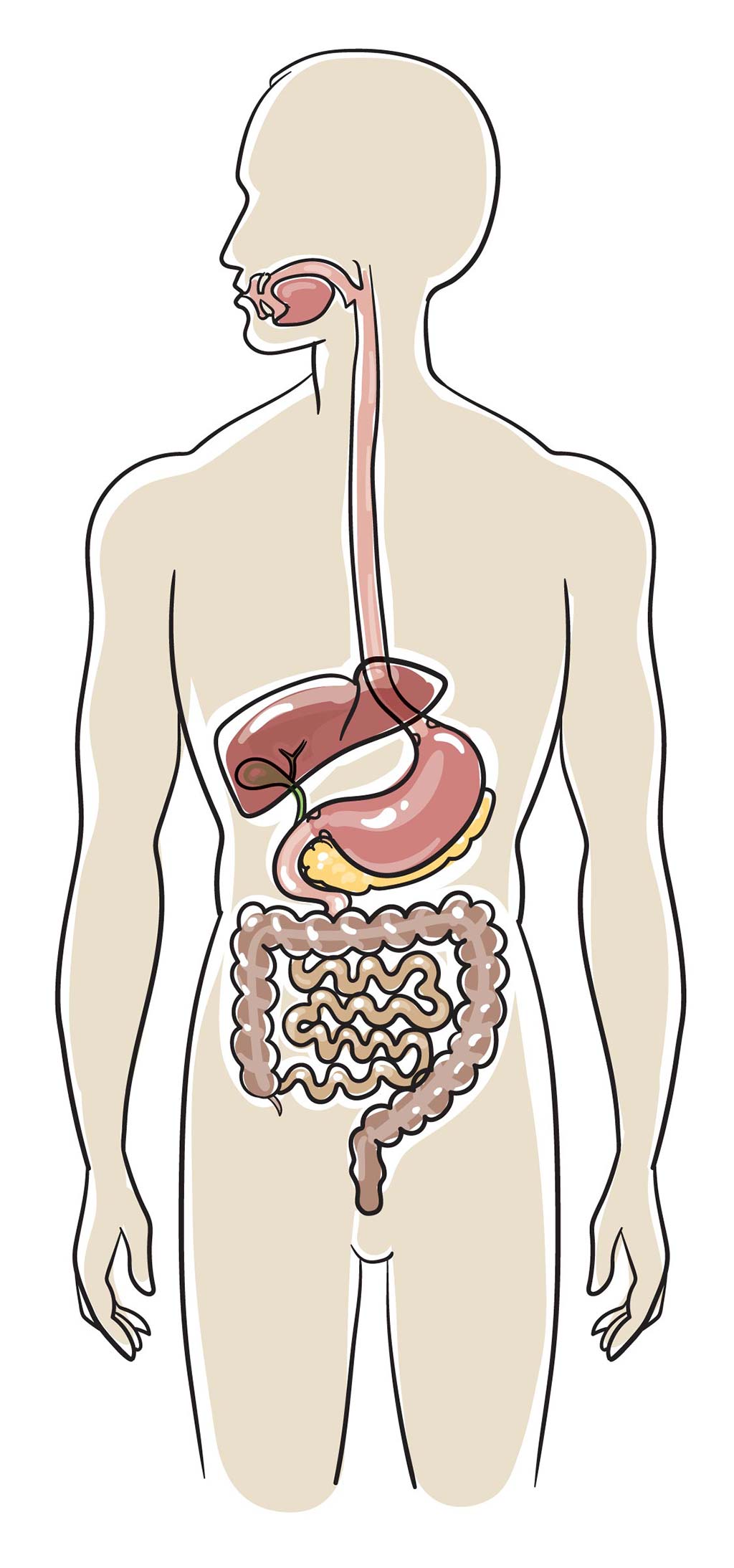
Stomach and intestinal (gastrointestinal) health
This fact sheet is for people who have had a blood and marrow transplant (BMT).
BMT patients may experience health complications in the months or years following the transplant. Long-term follow up has an important role in the early detection of any health issues.
This fact sheet has general information about ways to look after your health. If you have specific concerns, speak to your BMT team or your doctor for further information and advice.
What are the issues that could affect my gastrointestinal health after a BMT?
Gastrointestinal problems commonly occur during BMT. These can occur at any time, from pre-transplant preparation, to soon after a BMT and also in the months and years following BMT. They occur as a result of the effects of radiotherapy and chemotherapy, viral infection, graft-versus-host disease (GvHD) and medications used during BMT.
The most common gastrointestinal problems affecting long-term survivors of BMT include GvHD of the intestine or stomach, cytomegalovirus (CMV) infection, bacterial infection particularly due to Clostridium difficile, inflammation or ulceration of the stomach or intestine often due to medications including steroids and mycophenolate and cancer of the oesophagus or stomach, which although still rare occur more often in people who have had a BMT.
What are the symptoms?
Gastrointestinal problems may cause a range of different symptoms including
- diarrhoea or constipation
- stomach pains or cramps
- nausea or vomiting
- heartburn or indigestion
- bloating or gas
- feeling of fullness
- loss of appetite
- weight loss
- fever or chills.
How are gastrointestinal health issues diagnosed?
It is important that you speak with your BMT team about any symptoms you have. Gastrointestinal symptoms are often vague or non-specific and further tests are often needed to determine whether or not there is a problem and whether treatment is needed.
A number of different tests can be used to diagnose gastrointestinal problems.
- Blood tests including blood counts, liver tests and genetic tests for viral infection.
- Stool tests for infection.
- Gastroscopy or endoscopy – In this test a small flexible tube with a light and camera on the end is passed into your mouth, down your oesophagus, into your stomach and the first part of the small intestine so that the lining can be examined and biopsies (samples) collected.
- Colonoscopy or sigmoidoscopy – In this test a small flexible tube with a light and camera on the end is put up your bottom (anus), into your large intestine and the last part of the small intestine so that the lining can be examined and biopsies (samples) collected.
If a gastrointestinal health issue identified, how is it treated?
The treatment will depend on your individual situation.
Reflux, stomach inflammation or ulcers are generally treated with medications to reduce stomach acid and to protect the lining of the stomach or oesophagus.
Graft-versus-host disease is treated with steroids (e.g. prednisone and/or budesonide) and drugs that suppress the immune system (such as tacrolimus, cyclosporine and etanercept).
Infection is treated with anti-viral drugs or antibiotics.
Problems with absorption of food is treated with dietary modification and/or supplements and sometimes with enzymes to assist with digestion.
Whatever the problem is, medicines are always used to relieve symptoms and, where necessary, expert help is sought from other specialists including dieticians and gastroenterologists.
How can I look after my gastrointestinal health?
- Talk to your BMT team or general practitioner (GP) about any gastrointestinal symptoms you are experiencing.
- Ensure you take medications as prescribed, and tell your BMT team or GP if you are having difficulty taking your medication or experiencing any side effects from them.
- Make sure that you attend all your clinic appointments and have all your long-term follow-up tests.
- Ensure that you eat a healthy diet, limit your alcohol intake, do regular exercise and drink plenty of water – ideally more than more two litres each day.
- If you are able to, try and identify what foods make your symptoms worse and try to avoid them. You may need to be particularly careful with spicy, oily or fatty foods or dairy foods.
- Wash your hands regularly and maintain your personal hygiene.
- Know your ideal weight and try and maintain it. If you need to avoid becoming overweight or underweight, ask your BMT team or GP to refer you to a dietician to assist you manage your symptoms and make healthy choices.
Where can I find further information?
- National Health and Medical Research Council. Australian Dietary Guidelines. www.eatforhealth.gov.au
- Gastrointestinal Society of Australia. www.gesa.org.au
- The Australian Healthy Food Guide. Five golden rules of digestive health. www.healthyfoodguide.com.au