Collaboration and expertise from the Agency for Clinical Innovation’s (ACI) Mental Health Network, the health system, consumers and stakeholders is integral to the state's progress towards 'Zero Suicides in Care'.
The ACI is developing a suicide care pathway to support high-quality care for everyone with suicidal behaviours using NSW Health mental health services. The NSW Health Suicide Care Pathway is part of the Zero Suicides in Care (ZSiC) initiative, which is led by the Ministry of Health's Mental Health Branch. It provides a guide to suicide care interventions that services can use to:
- provide anyone with suicidal behaviours with a minimum set of interventions
- provide consistent and evidence-based care
- reduce unwarranted variation in service delivery across the state
- reduce suicides in care.
The ACI’s Mental Health Network is leading on developing the pathway and supporting local health districts (LHD) and specialty health networks (SHN) to implement localised pathways and build sustainable skills in this area.
Collaborating across the ACI and the health system
The pathway project is overseen by a working group chaired by Dr Andrew McDonald, the Director Clinical Services, Mental Health Services, Sydney Local Health District.
The stakeholders involved in the ZSiC project and development of the pathway include:
- Ministry of Health (Mental Health Branch)
- Clinical Excellence Commission
- Health Education and Training Institute
- The Zero Suicides Institute Australasia
- 15 LHDs and 2 SHNs
- Primary health networks
- The ACI’s Evidence directorate and Consumer Engagement and Redesign team.
People with lived experience of mental health services also play a central role in the project.
Why was the project established?
The pathway and other initiatives that make up the ZSiC project are part of the $87 million Premier’s Priority towards zero suicides. Coordinated by the Ministry of Health's Mental Health Branch, this initiative aims to reduce NSW’s suicide rate by 20% by 2023.
The pathway should ultimately provide a guide to the consistent and high-quality care anyone experiencing a suicidal crisis should expect to receive in NSW Health mental health services.
“Clinicians and consumers will be able to refer to the pathway to understand what effective care for people presenting with suicidal behaviours looks like,” explains Andrew.
What have been your major achievements so far?
To draft the NSW Health Suicide Care Pathway, the team referred to frameworks developed internationally, leveraged the experience of the health services who implemented them and collaborated extensively with NSW stakeholders.
“The draft pathway is now with LHD and SHN stakeholders, who will consult with their mental health clinicians and consumers over the next month,” explains Andrew. “Clinicians, services and health managers can use the draft to inform their work at present, while providing us with feedback for the finalised pathway, that will be published on the Agency for Clinical Innovation website.”
A Guide for Developing a Local Suicide Care Pathway document is also being produced. It will help LHDs and SHNs develop their own local pathways by incorporating key elements of the statewide pathway.
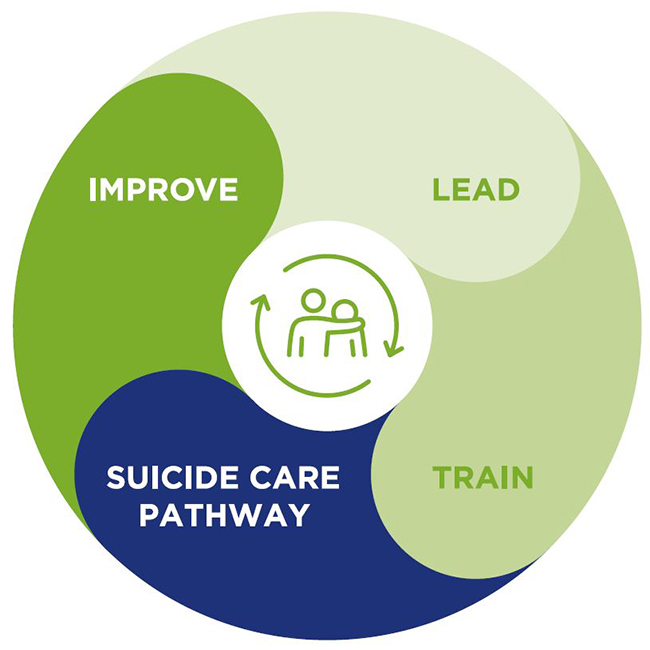
The ACI is leading on the suicide care pathway as part of the ZSiC project.
How do you maintain strong communication, collaboration and engagement with key stakeholders?
“Meeting up with key stakeholders on a regular and ongoing basis has kept momentum going,” says Deborah Howe, the ACI’s Mental Health Network Manager.
The network runs monthly meetings for the pathway working group and informal drop-in sessions for LHDs and SHNs. A ZSiC Community of Practice gets together to learn and share expertise. A fortnightly inter-agency ZSiC project team meeting helps keep projects on track.
What are your key focus areas over the coming months?
“We’re focused on supporting LHDs and SHNs to develop localised pathways based on the statewide model, using a co-design approach” explains Deborah.
“We’ll also be finalising the statewide pathway based on any feedback from consultation on the draft, and expect to have it published and available to everyone in early 2022.”
The project is due to be completed in June 2022. Join the network to stay up to date on their progress.
Tips for managing a project with multiple stakeholders
Deborah shares her top five tips for effective and collaborative project management.
- Work closely with key stakeholders, such as clinical and LHD project leads, to ensure project aims and deliverables are in line with the needs of clinicians, mental health staff and consumers on the ground.
- Establish regular and consistent meetings to foster a collaborative working space together.
- Encourage feedback and collaboration by telling your stakeholders why you value their insights. We do this by being authentic when we speak to our stakeholders, by acknowledging their expertise and by making ourselves available for informal discussions and feedback.
- Acknowledge where you need support, seek the expertise of others, and leverage your stakeholders and working groups.
- Follow through on what you say you're going to do.
October is Mental Health Awareness Month.