A new series of vignettes, as told by clinicians and health managers, share how Leading Better Value Care (LBVC) initiatives have been implemented locally.
LBVC is a key program accelerating value based healthcare across NSW Health. It involves clinicians, networks and organisations working together on high-impact initiatives to improve outcomes and experiences for people with specific conditions.
A new series of vignettes (or case studies) shines a light on local LBVC approaches to conditions such as bronchiolitis, heart failure, pulmonary disease, diabetes, hip fracture, osteoarthritis, osteoporosis, renal supportive care and wound care.
The vignettes highlight the organisational model of care used; what is special about the way care is delivered that is valuable for others to know; key lessons learnt; and related links and resources. They help clinicians and managers understand how local implementation can help them provide better value care for patients.
Gathering local knowledge and experiences
In 2019, the ACI published clinical priorities and organisational models for its LBVC initiatives. They provide clinicians with a quick reference to the key priority areas for change, and different approaches to implement the changes.
“The vignettes came about as a result of this work, as well as a crowdsourcing challenge to gather examples that demonstrate how care is being organised in different settings and contexts in NSW,” explains Tara Dimopoulos-Bick, one of the ACI’s Evidence Generation and Dissemination Managers.
The crowdsourcing resulted in more than 70 descriptions of local examples of LBVC implementation, with around 55 unique descriptions as told by clinicians and health managers fashioned into vignettes. The ACI has published the first batch of 20 approved vignettes. Each of the 10 LBVC initiatives supported by the ACI is illustrated in at least one vignette.
The vignettes are a wonderful opportunity to share knowledge and learnings across NSW Health.
“Crowdsourcing leverages the collective intelligence of online communities,” explains Tara.
“Sourcing local descriptions of organisational models and examples of local LBVC implementation proved an effective way to reach and engage with diverse audiences.
“It enabled the ACI to capture unpublished material as a form of organisational and experiential evidence, that can sit alongside and enhance the scientific evidence that supports the LBVC program.”
“The vignettes are a wonderful opportunity to share knowledge and learnings across NSW Health,” says Margaret Kelly, the ACI’s LBVC Implementation Manager.
Senior Podiatrist and High Risk Foot Service Coordinator, Emma Martin, contributed an LBVC story for diabetes high risk foot services in the Hunter New England Local Health District.
The outpatient clinic for diabetes high risk foot services opened at Tamworth Hospital in July 2018. It covers rural locations spread across a vast geographical distance, and one of the largest Aboriginal populations in NSW.
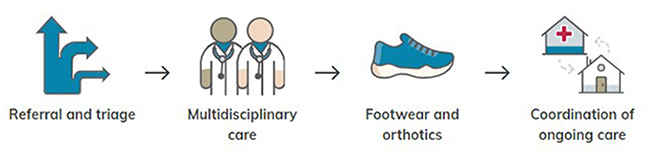
Organisational model used by the Tamworth Hospital service.
Emma explains how the clinic provides a multidisciplinary team approach to staffing that reduces the need for patients to travel extensively.
“Patients do not need to travel to Sydney or Newcastle for ongoing care, which saves them travel and accommodation costs. It also allows for patients to be treated closer to home.”
The vignette highlights these key lessons learnt for others:
- building personal relationship with patients makes a meaningful impact on staff
- establish a great network – networking and education throughout the district has been pivotal
- completing an Aboriginal health impact statement and displaying artwork by local indigenous artists.