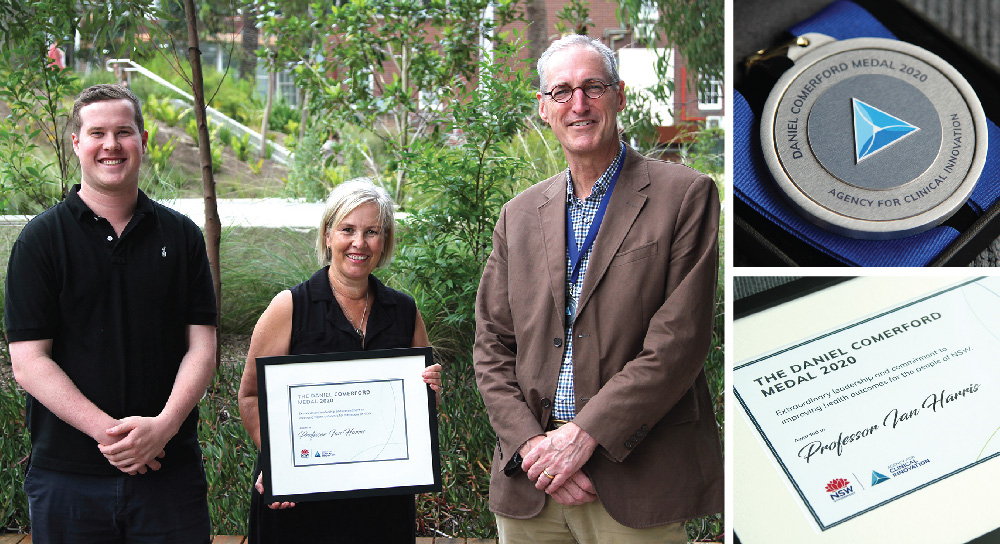
Orthopaedic surgeon and clinical academic, Professor Ian Harris reflects on receiving the inaugural Daniel Comerford Medal, which has reinforced his pursuit to make surgery (and medicine in general) more reliant on high quality evidence.
To my surprise and great honour, I received the inaugural Daniel Comerford Medal from the ACI in December last year. To receive an award named after someone who gave so much to the ACI and to improving clinical care was humbling and caused me to reflect on why I might have been chosen.
I have been in clinical practice as an orthopaedic surgeon for 25 years, and the last half of that has been spent as a clinical academic. I did not start as a surgeon aiming to change the practice of others, but merely to follow, or at least try to keep up. It was only once I learned the science of medicine (what is referred to as “evidence-based medicine”) that I could both appraise the research better and perform my own research.
After seven years in practice, I went back to university and have been a student, on and off, since then. Learning how to assess the evidence behind what we do as surgeons (and doctors in general) raised more questions than it answered, because I realised how weak the evidence was for many common practices. Many practices (including surgical operations) were being performed simply because that’s what our teachers did; and where high quality research had been performed, many procedures were of little or no benefit to patients.
It became my goal to study and expose the evidence supporting surgical procedures, particularly where the evidence showed them to be ineffective or where there was a lack of evidence.
I have since conducted many studies into surgical procedures, and studied the evidence for many others, focusing on the patient’s response to the treatment. For example, one of the most common surgical procedures in the world (and certainly in my field of orthopaedic surgery) is knee arthroscopy. This involves keyhole surgery, usually to clean up wear-and-tear in the knee, either the lining of the joint or the menisci (cartilages) that lie between the two bones. This procedure became popular in the later part of the 1900s, but it was not until early this century that high quality studies were performed. These studies consistently showed that the procedure was no better than non-surgical alternatives (like physiotherapy), and no better than pretending to do the procedure (placebo operations that didn’t involve any real surgery).
I was not surprised to learn that the procedure didn’t work, but I was very surprised to see that the rates of surgery were still rising, and that many surgeons didn’t believe, or weren’t aware of, the evidence. However, practice eventually changed and the rates of this type of surgery have been falling since 2011 due to the work of many people worldwide pushing this evidence-based approach.
I am lucky to have had a part in this push, by contributing to a large review of all studies in this area, and by looking at local practice change in NSW. I was able to publish how hospitals in NSW have responded to the evidence and changed practice. This research would not have been possible without support from NSW Health, including many who are now working at the ACI.
My main aim is to make surgery (and medicine in general) more scientific: less reliant on tradition and personal opinion, and more reliant on high quality evidence.
Receiving the Daniel Comerford Medal has reinforced my enthusiasm to maintain my work to increase the scientific basis for medicine.
About Professor Ian Harris
 Ian Harris is Professor of Orthopaedic Surgery at UNSW Sydney. He is based at Liverpool Hospital, where he has a clinical practice and conducts research through the Whitlam Orthopaedic Research Centre and the Ingham Institute for Applied Medical Research; and Royal Prince Alfred, where he conducts research through the Surgical Outcomes Research Centre (SOuRCe) and the Institute for Musculoskeletal Health. He is also the Clinical Co-Chair of the ACI’s Musculoskeletal Network.
Ian Harris is Professor of Orthopaedic Surgery at UNSW Sydney. He is based at Liverpool Hospital, where he has a clinical practice and conducts research through the Whitlam Orthopaedic Research Centre and the Ingham Institute for Applied Medical Research; and Royal Prince Alfred, where he conducts research through the Surgical Outcomes Research Centre (SOuRCe) and the Institute for Musculoskeletal Health. He is also the Clinical Co-Chair of the ACI’s Musculoskeletal Network.