This page is to assist clinicians to navigate the website and to implement a pain management plan.
What is the Chronic Pain and Brain Injury Website
Chronic pain is common after a brain injury, but it doesn’t need to stop people experiencing pain from living their lives. With the support of clinicians and carers, and through the use of simple, targeted tools, people with brain injury can learn to manage their pain. The Chronic Pain and Brain Injury Website provides a platform for these tools, and for a range of resources and information to support consumers, carers and clinicians to manage this complex condition.
The website was specially designed for people with a moderate-to-severe traumatic brain injury. It provides a framework to build understanding of chronic pain as well as tools for assessing and managing pain. The website has been designed for use by consumers with the support of a carer or clinician.
The website was developed by the Agency for Clinical Innovation (ACI), with funding from icare. It uses evidence-based principles, to give clinicians the tools to work with consumers to manage their pain.
How to use the Chronic Pain and Brain Injury Website
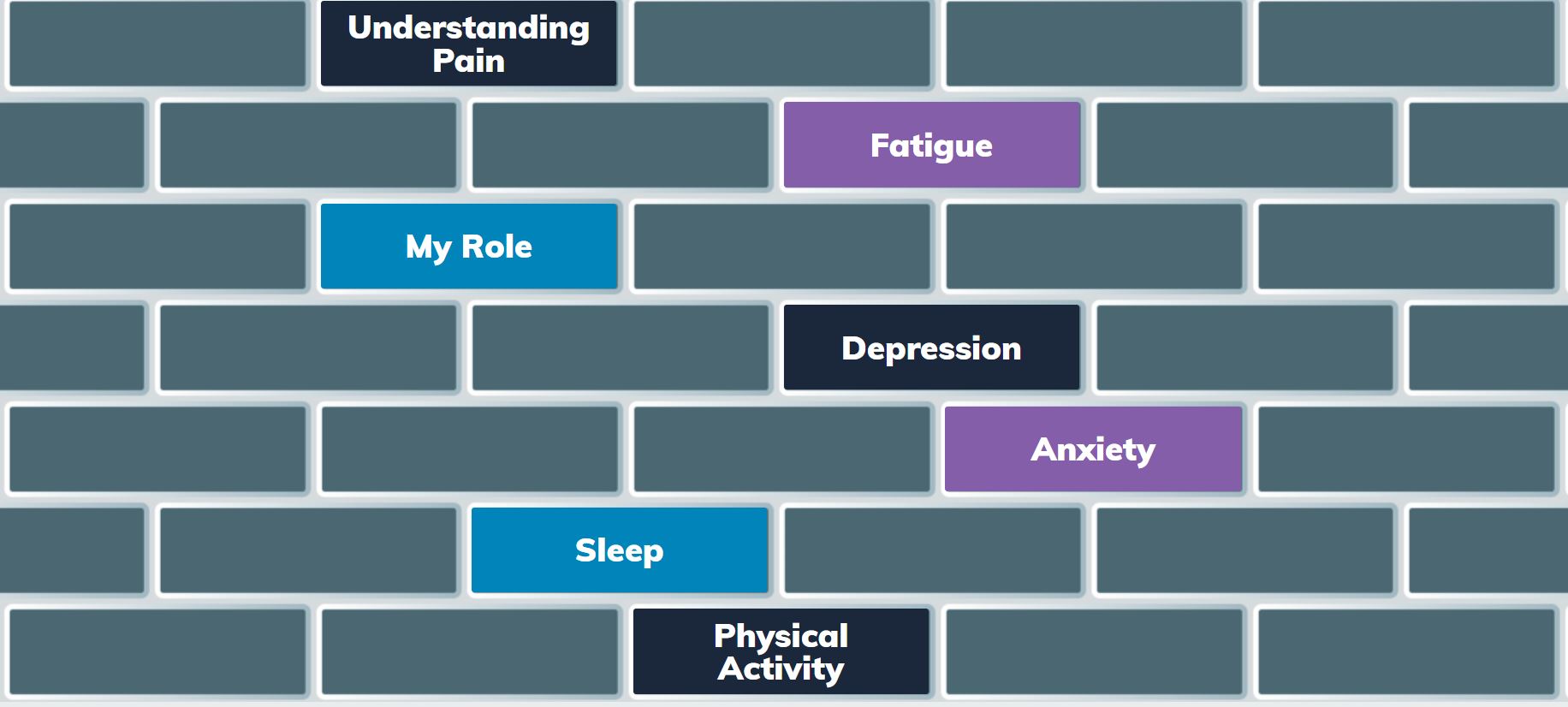
The brick wall was used as an analogy and clinical framework for the resources, providing users (consumers, carers and clinicians) with a clear structure to assess, use the appropriate tools and to make a pain management plan. The domains from the Patient Reported Outcome Measurement Information System (PROMIS®) were used to categorise the resources and to help users to prioritise which domain to access first. The resources are broken into seven bricks or categories:
- sleep,
- fatigue,
- my role,
- physical activity,
- depression,
- anxiety and
- pain.
These mirror the seven domains of the PROMIS® and are also key concepts used in chronic pain management.
Once you click on a brick, there is a brief description of how pain impacts this domain and how the person with pain could benefit from understanding more about this brick. Watch the short video to learn tools and tips about this brick.
Within each of the bricks, users can access six tips – these are brief hints and prompts that can immediately be used to help manage pain. Every time you use the website with a consumer, show them these tips to reinforce simple steps they can do to manage their pain.
Once you click through all the tips, each brick has six treatment tools, that are more in-depth strategies to enable the clinician to assist the consumer to learn specific pain management skills that they can employ in their everyday life. There are in 89 downloadable pdf pain resources for users to access. You can use the treatment tools individually or you can develop a Be Pain Smart Plan.
There is also a More Resources section which provides links to additional resources on that topic from a general pain management or brain injury perspective.
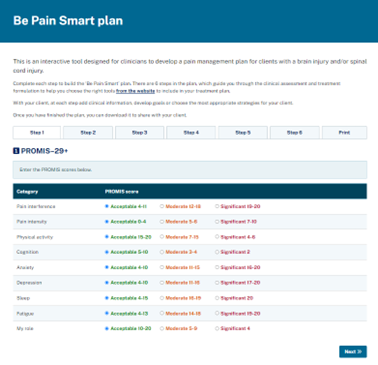
How to make a Be Pain Smart Plan
Developing an individualised pain management plan with someone with a brain injury is crucial to helping them to manage their pain. The Be Pain Smart Plan is an interactive online tool designed to assist clinicians with developing a personalised pain management plan with a person with a brain injury.
The plan has six steps to guide the clinician through the clinical assessment and treatment formulation, and to help choose the right tools from the website to include in the plan. With the consumer, at each step the clinician can add clinical information, develop goals or choose the most appropriate strategies.
Once the plan is finished, it can be printed and/or downloaded to share with the consumers and the rest of their team
Click here to develop a Be Pain Smart Plan.
Steps in the Be Pain Smart Plan
Select the icons below to see more information for each step.
Interested in learning more about how to manage chronic pain after a brain injury?
Register for The Be Pain Smart - Online Education Modules
This is a free online training program for clinicians to help build clinical skills in chronic pain management for people with a brain injury. There is also a module on managing pain after spinal cord injury. In a self-paced, online format, over 10 modules clinicians will learn:
- how to modify their pain assessment for people with a brain injury,
- how to develop an individualised pain management plan, and
- skills to implement pain management strategies modified for people with a brain injury.
It is perfect for clinicians and case managers who work with people with brain injury or spinal cord injury who want to know how to implement the resources on the website into their clinical practice.
Click here to register for the Be Pain Smart - Online Education Modules.
Spinal Cord Injury and Pain Management resources
If you would like to learn more about chronic pain after spinal cord injury (SCI) – click here to go to the Spinal Cord Injury Pain resources on the ACI Pain Network website.
The Spinal Cord Injury Pain Quicksteps is an interactive online tool to help a clinician build a pain management plan for a person with a SCI. It includes SCI and pain red flags, links to resources, and guides a clinician through all the steps involved in making a personalised pain management plan. Once finalised the plan can be downloaded and saved as a pdf.
More details about the Be Pain Smart Plan Steps
Step 1: Using the PROMIS®
PROMIS® stands for 'Patient-Reported Outcomes Measurement Information System'
The PROMIS® profiles are a set of person-centred measures that evaluate and monitor physical, mental, and social health in adults and children. This measure was identified as the most suitable patient-reported measure, to serve as a convenient and appropriate screening tool for monitoring the level of interference of pain for people with a brain injury. The tool has a fixed number of items from seven PROMIS® domains: depression, anxiety, physical function, pain interference, fatigue, sleep disturbance and ability to participate in social roles and activities (My Role).
Click here to learn more about how to use the PROMIS® and chronic pain after a brain injury.
Adults
- Download the PROMIS-29+ adult screening guide for more detailed information about how to use, score and interpret the PROMIS-29+ as a screening tool.
- Download this Spinal Cord Injury version of the PROMIS-29+ as a screening tool for people who have a SCI. In consultation with consumers and clinicians, the PROMIS-29+ was adapted for people with a spinal cord injury. The questions from the physical activity domains were excluded to accommodate different physical capacity – all remaining items of the questionnaire were unchanged.
Children
The PROMIS–25 has child and parent proxy versions, for use with children aged 5 to 17 years.
- Download the PROMIS–25 self-report screen guide for more detailed information about how to use, score and interpret the PROMIS–25 as a screening tool.
- Download the PROMIS–25 self-report form (child or young person: 8 to 17 years).
- Download the PROMIS–25 parent proxy form (child or young person: 5 to 17 years who is unable to complete the survey themselves).
Watch this video to learn how to use the PROMIS® as part of your Be Pain Smart Plan.
Step 2 - Clinical Assessment
When assessing someone with chronic pain after a brain injury, a clinician will need to adapt their assessment in order to examine the person's functional, physical, cognitive and psycho-social capacity and impairments. The Be Pain Smart Plan provides spaces to identify the biopsychosocial impairments/limitations or supports/resources which may impact on your pain management plan.
Watch this video to see overall principles to adapt a pain assessment for someone with a brain injury.
Watch this video to see how a physiotherapist would adapt their pain assessment.
Watch this video to learn how a psychologist would adapt their pain assessment.
Step 3 - The Brick Wall Exercise
When people have chronic pain, it can feel like their pain is holding them back from what they want to do and from meeting their goals. Often people feel like there is a big wall of pain in front of them, blocking them from getting to where they want to be. Clinicians understand though that pain is not the only barrier.
The Brick Wall exercise can be a helpful way to assist consumers to see the individual barriers (bricks) that are blocking them from reaching their goals. The exercise can help the person to see that the wall, is made up of different bricks; smaller parts that come together to create the wall.
The first step to breaking through the brick wall is help the person with pain, work out what are the bricks in their wall, that is, identify the problems and barriers in their life.
This is an invaluable tool for consumers to recognise the huge significance of pain in their lives and the breadth of barriers that they face. Visually seeing this can be a powerful moment and can highlight why they need a multi-disciplinary approach and why they more than just medications to manage their pain.
Clinicians can help consumers figure out “What are the bricks in their wall?” by using The brick wall of pain worksheet .
Watch a training video on how to do The Brick Wall exercise.
Step 4 - Select three priority bricks
A clinician can select the three priority bricks to initially work on, by using the results from the first three steps of the Be Pain Smart Plan and by helping the person with pain to identify the areas important to them. Often there will be themes that resonate through the PROMIS® results, clinical assessment and brick wall exercise, which will guide the initial brick selection.
Often starting with the ‘Pain’ brick can be a good opportunity to provide pain management education and this will help to provide a framework for using the tools in the other bricks.

Step 5 - Set Goals For Each Brick
Clinicians can use SMART goal skills to develop a goal for the three bricks selected in Step 4. Go to the Goal Setting page on the website to see how to use the SMART goal setting approach with chronic pain after brain injury.

Step 6 - Select two tools for each brick
The final step is to select two different treatment tools from each of the bricks selected in step 4 to work on with the person with pain.
Once the tools are selected, the Be Pain Smart Plan can be printed or saved as a pdf document.
Each treatment tool within each brick is listed below.
| Bricks | Understanding Pain | Fatigue | My Role | Depression | Anxiety | Sleep | Physical Activity |
|---|---|---|---|---|---|---|---|
| Tools | What is chronic pain | Doing more | Coming to terms with your pain | Noticing your thoughts | Worry time | Sleep diary | Doing more around your home |
| Pacing | Noticing your thoughts | Adjusting to the new you | Changing your thoughts | Relaxation | Sleep practices | Getting up and getting ready | |
| Lifestyle and Nutrition | Boom and bust | Getting back into the community | Common unhelpful thoughts | Noticing your thoughts | Bedtime routine | Getting back into leisure | |
| Goal Setting | Pacing | Communicating better | Managing my emotions | Calming down | Meditation | Getting out and about | |
| Maintaining the changes | How to recharge | Changing roles | Cycle of depression | Winding down your stress | Sleep and worry | Pacing | |
| Flare-ups | Lifestyle and nutrition | Repairing relationships | Managing your thoughts | Building but-by-bit | Sleep thought swaps | Getting more active |