Toolkit
Pressure Injury Toolkit For Spinal Cord Injury and Spina Bifida
Beyond the wound - Bringing best practice to the bedside

Stage
Wound Assessment Stage
Images reproduced with permission of AWMA. All rights reserved.
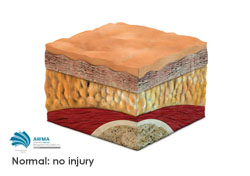
Normal Skin
- Skin is our body’s largest organ
- Skin is 0.3-3mm thick, consisting of layers; Epidermis, Dermis, Subcutaneous
- The function of the skin is for protection, sensation, thermoregulation, excretion, secretion, synthesis of Vitamin D
- The condition of the skin often reflects a person’s overall state of health.
- Good skin health increases tolerance to external forces and reduces the likelihood of skin breakdown.
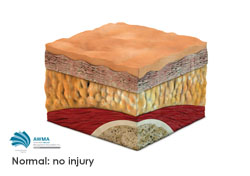
Image Credit: Reproduced with permission of Wounds Australia . All rights reserved.
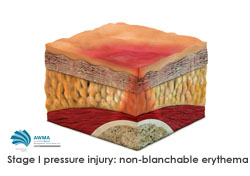
Stage 1
- Intact skin with a localised area of non-blanching redness, usually over a bony prominence.
- Redness persists > 20 mins after relieving pressure.
- NB: Darkly pigmented skin may not have visible blanching, but colour may differ from the surrounding area.
- The area may be painful, firm, soft, warmer or cooler than adjacent tissue.

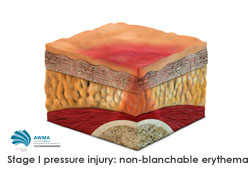
Image Credit: Reproduced with permission of Wounds Australia . All rights reserved.
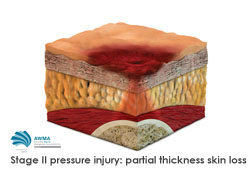
Stage 2
- Partial thickness loss of dermis presenting as a shallow open wound with a red-pink wound bed.
- May present as an abrasion or a serum-filled blister (may be intact or open/ruptured).
- The epidermis and possibly the dermis will be breached.
- Presents as a shiny or dry shallow ulcer without slough or bruising.
- NB: not skin tears, tape burns, perineal dermatitis, maceration or excoriation.
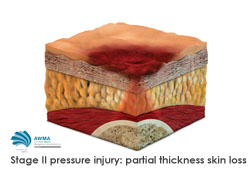

Image Credit: Reproduced with permission of Wounds Australia. All rights reserved.
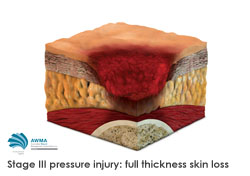
Stage 3
- Wound extending through epidermis and dermis into the fatty subcutaneous layer.
- Subcutaneous fat may be visible, but bone, tendon or muscle are not exposed.
- Slough may be present but does not obscure the depth of tissue loss.
- May include undermining or tunnelling (NB: Undermining is a separation of tissue beyond the wound margin.)
- The actual depth of a stage III pressure injury varies by anatomical location.
- Refer to tertiary service. See NSW SSCIS Pathway for Management of PI in SCI
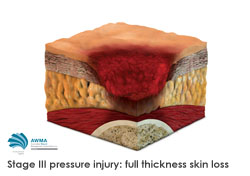

Image credit: Reproduced with permission of Wounds Australia. All rights reserved.
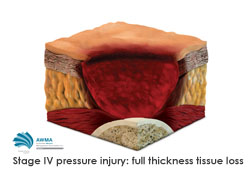
Stage 4
- Full thickness tissue loss extending into underlying tissues such as muscle and possibly bone.
- Visible or palpable exposed bone, tendon or muscle.
- Slough or eschar may be present on some parts of the wound bed.
- Extension to muscle, tendon or joint capsule increases the risk of osteomyelitis. See Complications of would healing for more information.
- The depth of a stage IV pressure injury varies by anatomical location. For example a relatively shallow wound overlying the Achilles tendon or 5th metatarsal head, may progress rapidly to a stage IV if pressure is not removed rapidly after early signs of developing a pressure injury.
- May include undermining and sinus tracts.
- Refer to tertiary service. See NSW SSCIS Pathway for Management of PI in SCI
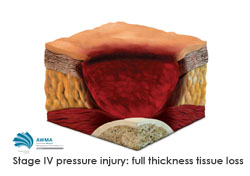

Image credit: Reproduced with permission of Wounds Australia. All rights reserved.
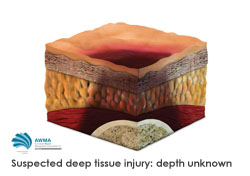
Deep tissue injury
- Purple or maroon localised area, an area of discoloured intact skin, or a blood filled blister.
- Deep tissue injury (DTI) is due to damage to the underlying soft tissue from pressure and/or shear forces.
- The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue.
- DTI may be more difficult to visually detect in people with darker skin tone. Gently palpate suspected areas.
- Evolution may include a thick blister over a dark wound bed. The PI may further evolve and become covered by thin eschar. Evolution may be rapid exposing additional layers of tissue even with optimal treatment.
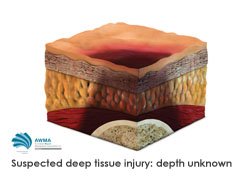

Image credit: Reproduced with permission of Wounds Australia. All rights reserved.
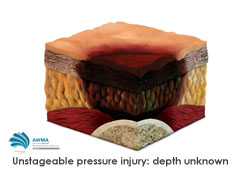
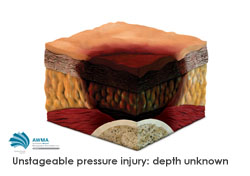
Unstageable
- Full thickness tissue loss in which the base of the pressure injury is covered by slough or eschar.
- Slough: colour yellow, tan, grey, green or brown.
- Eschar: colour tan, brown, or black.
- Until enough slough/eschar is removed to expose the base of the pressure injury, the true depth is not known, and therefore the stage cannot be determined.
- Stable (dry, adherent, intact without erythema or fluctuance) eschar on the heels serves as the body’s natural biological cover and should not be removed.