Cause and contributing factors - Assessment
SCI AND SB-specific factors and other medical conditions
Screen SCI and SB-specific factors, such as the following:
- Level and extent of SCI impairment
- Previous Pressure Injury
- Ageing
- Autonomic Dysreflexia
- Bladder and bowel incontinence
- Cardiometabolic Disease
- Heterotopic ossification or fracture
- Poor Nutrition
- Psychological / Mental Health Disorder
- Shoulder / upper limb pain and injury
- Spasticity and contracture
Comprehensive assessment of SCI and SB-specific and other medical conditions
Comprehensive assessment of SCI and SB-specific and other medical conditions
Cause and Contributing factors
| FACTOR | INFORMATION |
|---|---|
Level and extent of SCI impairment | Impaired movement and sensation increases risk of developing a pressure injury (PI), with the highest risks for individuals with complete SCI lesions, who have muscle paralysis with no sensation below level of injury. A vertical or transverse extension of the spinal lesion due to late syringomyelia causing further sensory or motor impairment will increase PI risk, and if clinically suspected should be investigated with a MRI scan of the spine. |
Previous Pressure Injury | A history of PI significantly increases the risk of developing further PIs in the future. Important information to record includes location, date, time to heal, likely cause and how PI was managed. These factors may influence your choice of treatments in the future. |
Time since injury | PI risk increases as time since injury increases to 10 years or more, being related to a combination of autonomic dysfunction, cardiovascular and metabolic changes, muscle wasting, musculoskeletal overuse affecting ability to transfer, and skin ageing process, as well as chronic conditions, such as obstructive sleep apnoea (OSA). |
Acute illness | An acute illness in a person with SCI or SB may increase PI risk due to compromised ability to undertake normal protective skin behaviours or self-direct care, inadequate nursing care or equipment (eg. alternating air cell mattress), reduced awareness / level of consciousness (see below), altered physiology (eg. hypotension, hypovolaemia, reduced tissue perfusion / oxygenation), or patients who experience weight loss (eg. nil-by-mouth over extended period). |
Ageing | Age-related changes can increase the risk of a PI due to thinning of skin and collagen with loss of skin strength and elasticity, reduced muscle mass and musculoskeletal changes with ageing impacting on mobility. |
Autonomic Dysreflexia | This is a Medical Emergency - see Red Flag . Autonomic Dysreflexia (AD) occurs in persons with a SCI at/above mid-thoracic level in response to a noxious stimulus below the level of injury, and is characterised by sudden onset of high blood pressure, pounding headache, flushing and profuse sweating above level and pallor below SCI level. Consider PI as a cause in context of prolonged or recurrent AD without another obvious cause. |
Bladder and bowel dysfunction | Urinary or faecal incontinence may contribute to PI through moisture, dermatitis and possible bacterial infection of wounds. A continence assessment must be included as part of any pressure injury assessment process for people with SCI to optimise treatment and healing. Prolonged bowel routines (> 1 hour) may also expose the skin to regular periods of high pressure on the toilet or commode chair and may be considered as a causative factor in PI development. |
Cardiometabolic Disease (CMD), Peripheral Artery Disease (PAD), Diabetes | CMD, PAD and diabetes are associated with poor wound healing. PAD in people with SCI may be more difficult to diagnose as pain and leg cramping (claudication) can be masked. PAD can be diagnosed using the ankle-brachial index (ABI) test, doppler ultrasound, magnetic resonance angiogram or CT angiography.20 |
Cognitive Impairment | Known cognitive impairment (TBI or SB with hydrocephalus), dementia, acute delirium from illness, confusion or sedation from high doses of medications (eg. opioids), or other conditions, place the person at higher risk of a PI. Identify persons with impaired cognition based on history and screen for dementia in those aged 65 years and older, so that a management plan can be instituted. |
Heterotopic Ossification | The formation of bony tissue in soft tissue where bone does not normally exist is not uncommon in individuals with SCI or SB. Heterotopic ossification (HO) can restrict joint range of motion cause joint contracture (eg. around knees, hips, elbows, shoulders) and exacerbate pain, and therefore may increase propensity to developing a PI through difficulty in completing self-care activities, performing transfers and weight shifting, and inability to adopt appropriate postures (supine and sitting) for effective pressure redistribution. HO can also form additional bony prominences that can create abnormal pressure points and PI risk or ectopic bony tissue within a chronic wound that may form the nidus of osteomyelitis. HO should be investigated (X-ray, bone scan), particularly if surgical intervention for a PI is being sought. Whilst X-ray is highly specific in the diagnosis of HO, it lacks sensitivity in early diagnosis. |
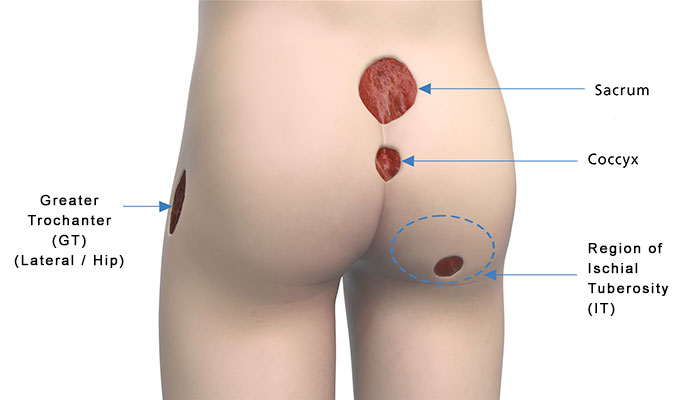
Leg fracture | An individual with a fracture in the lower limb is at an increased risk of PI; first, on the side of fracture due to immobilisation in rigid casts or splinting materials, which may cause pressure and second, over the ischial tuberosity (IT) or another part of the bottom if the leg is elevated when sitting, whereby pressure is increased over the IT. |
Pain | Pain is common after SCI and may affect a person’s ability to perform daily mobility tasks, and can affect mood, participation and quality of life. Neuropathic pain may increase as a result of a noxious stimulus below the level of SCI, such as PI, HO, trauma, and so on. See the ACI Chronic Pain website for more information. |
Poor Nutrition | Nutrition plays a vital role in PI prevention, as well as wound healing. Abnormal nutritional biomarkers may indicate an increased risk for PI; for example anaemia; low serum pre-/albumin. Screening with routine blood tests/biochemistry in conjunction with review of oral intake of food and fluids (ie. adequacy of nutrition), may help to reduce PI risk and provide evidence for early dietitian referral and implementing nutritional support when indicated. |
Psychological / Mental Health Disorder | The presence of a psychological or mental health disorder, such as depression or alcohol and substance abuse, may adversely impact on a person’s ability to self-manage, risk awareness/insight, problem solving ability and contribute to poor motivation, neglect and disengagement in self-care activities. The Emotional Wellbeing Toolkit: A Clinician’s Guide to Working with SCI provides a number of brief standardized tools to help clinicians to assess issues such as mood, anxiety, pain, trauma, substance use and psychosis. |
Respiratory complications | Respiratory function is often compromised after SCI, particularly in persons with tetraplegia or higher levels of paraplegia, with reduced lung volumes, difficulty expectorating secretions and an increased risk of developing acute respiratory complications, as well as a high incidence of chronic Obstructive Sleep Apnoea (OSA). Additionally, pneumonia is a risk factor for PI development after SCI, and individuals on bed rest for PI are also at an increased risk of developing pneumonia. |
Shoulder / upper limb pain and injury | Trauma to the upper limb affects an individual’s ability to safely lift and transfer their body weight throughout the day. This increases PI risk due to the potential for trauma, friction, shear and pressure forces occurring when the person with SCI or SB is unable to effectively lift their body weight for clearance and transfer safely. |
Spasticity and contracture | Muscle spasticity is common after SCI. Spasticity can be protective by helping to maintain muscle bulk and improving blood flow in paralysed limbs. However, excessive spasms can also cause friction and shear forces, contributing to PI development or delayed healing of a PI, and should be part of a comprehensive assessment and ongoing management of a PI in a person with SCI. |
Smoking | Smoking increases the risk of developing a variety of health complications, including respiratory complications and cardiovascular disease. In addition, smoking reduces blood flow and delays wound healing. |
Nutrition
People with SCI or SB and a PI are nutritionally at risk and should be screened routinely by the attending health professional. The Malnutrition Screening Tool (MST) either as a stand alone tool or performed as part of the Waterlow Score, should be performed by a member of the treating team. Scores ≥ 2 require dietitian referral for comprehensive nutritional assessment.
Comprehensive Nutritional Assessment20,51
Refer to a Dietitian for a comprehensive nutritional assessment which includes:
Anthropometric measures: Height, weight, recent unintentional weigh gain or loss.
Physical examination:Evidence of subcutaneous fat losses and muscle wasting related to malnutrition.
Biochemistry: Electrolytes, Creatinine, Pre-albumin, Albumin, Total Protein, C-Reactive Protein (CRP), Haemoglobin, Transferrin, Iron, Vitamin B12, Folate, Zinc, Vitamin D and Cholesterol.
Clinical signs and symptoms: Chewing or swallowing difficulties; Drug/nutrient interactions; Gastrointestinal function, i.e. nausea, vomiting, diarrhoea, constipation, pain, reflux, anorexia; Functional capacity / fatigue; Psychological well-being – depression, anxiety; Oedema and /or oedema (related to malnutrition).
Dietary Intake: Food and fluid intake history; Ability to acquire and prepare food; Cultural influences
Estimated Nutrition Requirements: Energy; Protein; Fluid; Micronutrients.
Nutritional calculations should be adapted to meet specific needs of those with SCI
For children and adults with SCI or SB, Body Mass Index (BMI) alone is not a valid indicator of healthy weight or chronic disease risk.
Body Mass Index (BMI)
Use of Body Mass Index (BMI) alone is not valid in adults or children with SCI or SB. Individuals with SCI have higher fat mass than fat-free mass making BMI ranges unreliable, and modified estimates are recommended. There is evidence in the literature to adjust the height and weight tables by reducing ~5-10% in paraplegia and 10-15% on tetraplegia. i.e. paraplegia subtract 4.5-7kg and tetraplegia subtract 7kg-9kg from the guideline healthy weight to calculate estimated BMI for person with SCI.29
A BMI of ≥22 kg/m2 indicates obesity in the SCI population compared to a BMI of ≥30 kg/m2 in the general population12
Mechanical factors
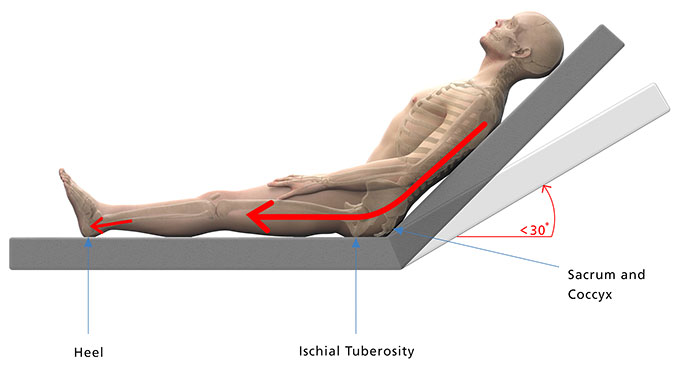
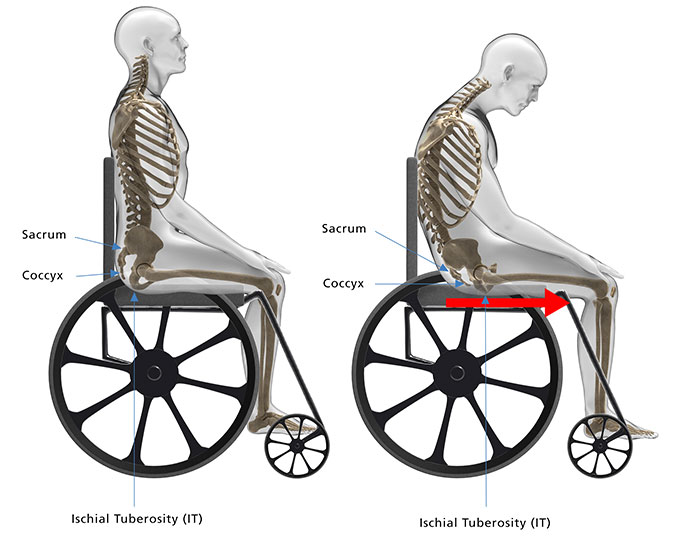
Shear
A shearing force occurs when the person’s body moves one way and the skin stays in place against the support surface. The movement causes shear stresses between the bony prominence and the overlying soft tissue.
It is important to be able to recognise a shear stress to adequately address contributing factors.
Reference
International review. Pressure ulcer prevention: pressure, shear, friction and microclimate in context. A consensus document. London: Wounds International, 2010
- Understand the person and how their SCI or SB impacts on their mobility, function and activities.20
- Screen for a change in function, mobility and mechanical factors by reviewing activity and equipment used throughout entire 24 hour period.20
- Refer to occupational therapist for Comprehensive 24 Hour Assessment.20
- Determine the cause of the pressure injury and contributing factors
- Develop an effective treatment plan
- Establish prevention strategies to reduce future PI risk.
- Consider mobility equipment e.g.: manual wheelchair, power wheelchair (whether it has a tilt in space function), pressure-relieving cushion, orthotics and duration of use of each of these mobility devices. Consider the age and how well maintained the equipment is.
- Children with SCI or SB quickly outgrow their equipment (including wheelchairs postural supports, TLSO back braces and Ankle Foot Orthosis (AFO)) and commonly experience postural asymmetry and changes due to scoliosis or limb contractures that increase their risk of PI from their equipment
- Look for shearing during re-positioning, or high pressure over bony prominences, is the mattress and bed adequate for the person’s current needs?
- Consider technique, types of transfers, equipment used, frequency, and total number per day.
- Children may rely on carers to transfer them safely. Their body or legs are at risk of being knocked and their skin may be at risk of friction or shear from dragging across the bed if slide sheets are not used.
- Consider balance, technique, assistance required
- Ask about bladder and bowel routines, equipment used, accidents, complications
- Assess technique used, frequency and duration of unloading, assess both beliefs and practices of pressure relief
- Consider if clothes have thick or hard seams are tight or are made from synthetic fabric.
- Children and adolescents will often choose clothing, underwear or footwear that is fashionable rather than what might be optimal for protecting their skin.
- Consider movements, transfers and equipment used when playing sport and participating in leisure activities.
- Consider the different surfaces the person is exposed to. Children will play and move around on the ground between hard surfaces, such as concrete, gravel, rocks, rubber playground flooring, plastic playground equipment, sand at the beach, and in sandpits. They may be at risk of insect bites from playing on the ground and heat burn from sliding on play equipment.
- Urgent hire, loan or permanent upgrade of pressure relieving equipment and additional personal care services is required during the healing AND recovery phase.
- Early referral to an occupational therapist, seating therapist and social worker or case manager is strongly recommended.
Comprehensive 24 Hour Assessment 20
Refer to an occupational therapist for a comprehensive 24 hour assessment.20
The Comprehensive 24 Hour Assessment includes positioning, mobility, function and support surfaces used by the person throughout the entire 24-hour period to determine the combined influence of these extrinsic factors.
A comprehensive assessment is essential to:
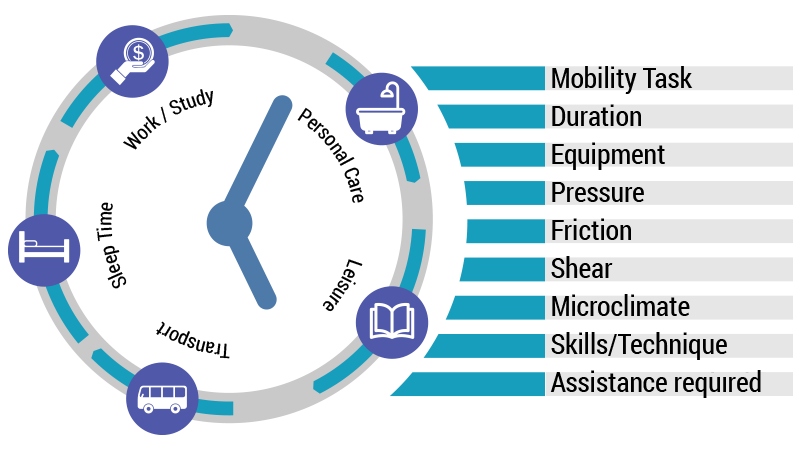
Consider forces such as pressure, friction, shear as well as microclimate with respect to:
Mobility
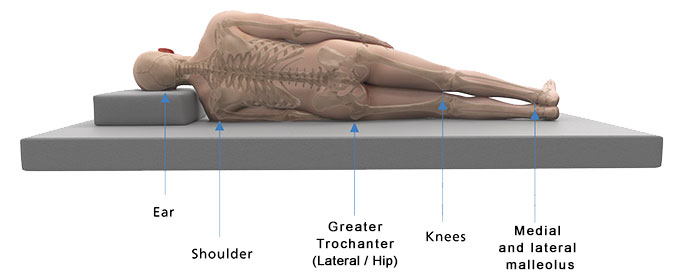
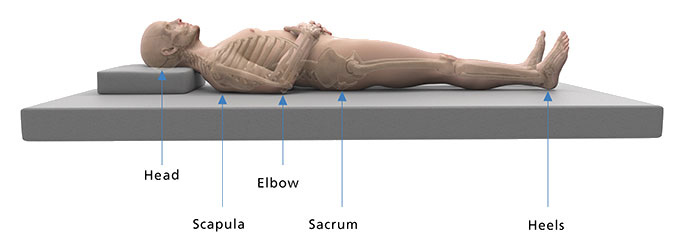
Positioning in bed
Transfers
Personal care and dressing tasks
Continence
Pressure Relief
Clothing and footwear
Sport, leisure and play
Reference
Houghton PE, Campbell KE and CPG Panel (2013). Canadian Best Practice Guidelines for the Prevention and Management of Pressure Ulcers in People with Spinal Cord Injury. A resource handbook for clinicians.
Psychological and mental health disorders
Psychological disorders require prompt attention and are associated with pressure injuries. Psychological disorders, negative self-concept and poorly managed anger can interfere with a collaborative approach to pressure injury management.11
Depression
Clinical Presentation
- Early morning awakening
- Altered appetite
- Significant weight change
- Reduced motivation +/- withdrawal from valued activities
- Depressed mood
Possible Diagnosis
Depressive disorder
Screening Tools
Referrals to Consider
- Psychologist
- Psychiatrist
- Also refer to GP to access Medicare rebate for psychology services
Consumer Resources
- beyondblue
- Mindspot. Treatment courses
- Mental Health Helpline: 1800 011 511
- Lifeline: 13 11 14
Substance Use
Clinical Presentation
- Interference with activities or reduced motivation +/- withdrawal from valued activities.
- High levels of alcohol or other illicit substance use
- Alcohol or drug use that is difficult to control and impacting on behaviour.
- Patient self report, or reported by significant others
Possible Diagnosis
Alcohol or substance use
Screening Tools
Referrals to Consider
- Psychologist
- Psychiatrist
- Drug and Alcohol service
- Also refer to GP to access Medicare rebate for psychology services
Consumer Resources
- beyondblue
- Mindspot. Treatment courses
- Mental Health Helpline: 1800 011 511
- Lifeline: 13 11 14
Exacerbation of pre-existing mental illness/disorder
Exacerbation of pre-existing mental illness/disorder
Clinical Presentation
- Exacerbation of a pre-existing mental illness may effect a person’s ability to carry out pressure injury prevention and contribute to pressure injury develop.
- Also, the experience of having a pressure injury may exacerbate a pre-existing mental illness such as anxiety or depression, as pressure injury management can cause social isolation, inhibit engagement with vocational or recreational activities and limit meaningful activity.
Possible Diagnosis
Exacerbation of pre-existing mental illness e.g. bi-polar disorder or schizophrenia
Screening Tool
Referrals to Consider
- Psychologist
- Psychiatrist
- Emergency Mental Health Team
- Also refer to GP to access Medicare rebate for psychology services
Consumer Resources
- beyondblue
- Mindspot. Treatment courses
- Mental Health Helpline: 1800 011 511
- Lifeline: 13 11 14
Psychosocial and lifestyle factors
Psychosocial and lifestyle factors contribute significantly to skin breakdown and impact on wound healing.
Screen for:
- Limited social support or living alone
- Inadequate personal care and/or domestic assistance
- Caregiver fatigue
- Financial concerns (Including access to quality equipment, repairs, provision of services)
- Unsustainable work or family commitments
And identify a person’s20
- Lifestyle priorities
- Perceived trade-off between pressure management requirements and living life
- Competing interests, roles and responsibilities
- Coping and problem solving strategies for preventing PI
- Fear of hospitalisation
Assessing psychosocial and lifestyle factors in SCI
Assessing psychosocial and lifestyle factors in SCI
“Psychosocial and lifestyle risk factors affect motivation and ability to adhere to essential skin care and pressure management strategies”.20
As part of a comprehensive psychosocial assessment, investigate the following predisposing factors20:
| Factor | Assessment Tools |
|---|---|
| Pain | ACI SCI Pain Navigator |
| Quality of life | SCIRE Project: Quality of Life Outcome Measures |
| Depression | See Psychological Disorder: Depression (above) |
Lifestyle factors
This table23 can be used by health professionals and consumers to explain pressure injury development and target risk factors. Information is based on results from the University of Southern California (USC) and Rancho Los Amigos National Rehabilitation Center (RLANRC)’s Lifestyle Redesign® for Pressure Ulcer Prevention in Spinal Cord Injury project.
| FACTOR | EXPLANATION |
|---|---|
| Perpetual danger | Even when an individual implements preventive strategies, unforeseen circumstances may trigger pressure ulcer development. |
| Change or disruption of routine | Development of a pressure ulcer may sometimes be traced to a single change that disrupts the existing risk equilibrium and produces a cascade of events. |
| Decay of prevention behaviours | Distractions, forgetfulness, and other factors may reduce the frequency of performing prevention techniques, often without the individual even recognising it. |
| Lifestyle risk ratio | This is the impact of the sum of physical or lifestyle liabilities, such as poor nutrition and inadequate finances, and buffers, such as a good support system and adherence to preventive strategies. |
| Individualisation | The unique balance of risk and prevention factors at any given time for each person with spinal cord injury determines pressure ulcer development. |
| Simultaneous presence of prevention awareness and motivation | Long-term prevention knowledge, short-term attention to the situation, and adequate motivation to perform the strategies must all be present to prevent pressure ulcer development. |
| Lifestyle trade-off | The ways in which an individual balances the needs to engage in personally meaningful activities and to use rest and caution to prevent pressure ulcers change the risk balance. |
| Access to needed care, service, and supports | The inability to obtain appropriate services, for various reasons, at the time they would be most beneficial or necessary increases pressure ulcer risk. |



 Consider:
Consider: