Acute low back pain
General resources
The below covers the following topics:
General Notes
Back to the top
Low back pain is a very common problem with approximately 80% of Australians suffering from back pain during their lifetime (1). Back pain can be a significant and debilitating condition placing a considerable strain on healthcare systems, with up to 35% of sufferers still experiencing problems after 5 years (2,3). However, with an early, effective and multidisciplinary approach to management, the rate of recurrence and long-term disability can be substantially reduced (2-5).
Only about 40% of those with back pain will seek medical advice and around 10% of those patients will have significant disability, with a proportion of these attending the Emergency Department (ED) (1,5,6). Such patients pose a significant burden to the ED accounting for up to 2% of all attendances and requiring an average length of stay between 4 to 5 hours (2).
The vast majority of patients with acute low back pain will have a non-specific musculoskeletal cause with a self-limiting course that will typically improve rapidly within a month and be fully resolved by 6 weeks. However, a minority (0.1-1%) of patients will have potentially serious spinal conditions such as fractures, tumours, spinal infections and cauda equina syndrome that require urgent diagnosis and management(1,5,6,7). Others may have significant non spinal causes of back pain including pyelonephritis, renal colic or abdominal aortic aneurysm that require just as urgent attention. These serious conditions can be identified in the initial assessment and examination by searching for the presence of any red flag features. - see acute low back pain - assessment.
If any red flag features are identified then a senior emergency doctor review should be sought to determine appropriate and timely investigations and management. If no red flags are identified patients should be commenced on a suitable multimodal analgesic strategy, reassured, educated, encouraged to mobilise (as tolerated) and referred to a physiotherapist early.
This clinical tool has been produced to provide a guide for the safe and effective management of adults with acute low back pain (pain for less than 4 weeks). Patients with persistent or subacute (pain for 4-12 weeks) or chronic low back pain (longer than 12 weeks) may require a more complex approach with consultation of multidisciplinary services such as rheumatology, pain specialists and neurosurgery.
Further References and Resources
Back to the top
- Walker, B.F., Muller. R. & Grant, W.D. Low back pain in Australian adults: prevalence and associated disability, J Manipulative Physio Ther, 2004; 27(4):238-44.
- Lovegrove, M.T. et al. Analysis of 22,655 presentations with back pain to Perth emergency departments over five years, International Journal of Emergency Medicine, 2011; 4:59.
- Chou, R. et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society, Ann Intern Med, 2007;147(7):478-91.
- Dahm, K.T. et al. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica, Cochrane Database Syst Rev, 2010;(6):CD007612.
- National Collaborating Centre for Primary Care. Low back pain: early management of persistent non-specific low back pain. NICE clinical guideline 88, London: National Institute for Health and Clinical Excellence 2009.
- Jarvik, J.G. & Deyo, R.A. Diagnostic evaluation of low back pain with emphasis on imaging, Annals of Internal Medicine, 2002; 137(7): 586-97.
- Goergen, S. et al. Acute Low Back Pain. Education Modules for Appropriate Imaging Referrals, Royal Australian and New Zealand College of Radiologists; 2015.
- Lavy, C. et al. Cauda equina syndrome, BMJ, 2009, 338:b936
- Capra, F. et al. Validity of the straight leg test for patients with sciatic pain eith or without lumbar pain using magnetic resonance imaging results as a reference standard, J Manipulative Physiol Ther, 3 May 2011, 24(4), 231-8.
- Murphy, D.R. et al. Pain patterns and descriptions in patients with radicular pain: Does the pain necessarily follow a specific dermatome? Chiropractic and Osteopathy, 2009; 17(9).
- Agency for Clinical Innovation, Management of people with Acute Low Back Pain: Model of Care, 2016.
Assessment
Back to the top
A thorough and structured initial history and physical examination is required to identify patients at risk of significant pathology that should prompt early senior doctor involvement and further investigation. Below is a list of red flag indicators that must be evaluated in the patient history and examination to alert us to potential serious diagnoses. If any of the red flag findings are identified, senior doctor input must be sought urgently to guide patient management and analgesia should be prescribed (see acute low back pain - treatment). The absence of red flag findings does not always exclude serious pathology.
Red Flags
- History of cancer
- Unexplained weight loss
- Severe pain when supine and/or at night
- Age <16 or >50 years
- History of significant trauma
- Intravenous drug abuse
- Recent bacterial infection or fever
- Immune suppression (HIV, transplant, corticosteroids)
- Saddle anaesthesia
- Bladder dysfunction (urinary retention or incontinence)
- Bowel dysfunction (faecal incontinence)
- Neurological deficit in either or both lower limbs (especially if progressive)
- Persistent symptoms for >4 weeks (recurrent presentations, worsening pain)
- Pregnancy
- Representation
After initial assessment it may be helpful to classify your patient into 1 of 4 broad categories to guide your decision making and management:
- Back pain with any red flags
- Urgent senior doctor involvement required as described above.
- Back pain with associated radiculopathy
- These patients have historical evidence of ‘sciatica type’ pain that radiates to either buttock or leg with no neurological abnormalities, indicating nerve root involvement.
- Dermatomal distribution (9) of the pain may reflect the nerve routes involved.
- Although the vast majority of these patients will experience symptomatic improvement or resolution within a month with appropriate analgesia and physiotherapy, earlier or more frequent re-evaluation by a general practitioner or spinal surgeon is advised.
- Non-specific musculoskeletal causes
- More than 85% of patients who present to ED with low back pain will have no specific cause found and will recover symptomatically within a month with appropriate analgesia and physiotherapy.
- Back pain from a non-spinal cause
- This category can be further subdivided into:
- Non-spinal conditions requiring urgent attention. Early senior doctor involvement to expedite diagnosis and definitive management (e.g. suspected ruptured AAA or those conditions bolded above – (see causes of acute low back pain).
- Non-spinal conditions requiring acute attention. The management of these conditions will not be discussed here, but will require appropriate care for the likely diagnosis (e.g. pyelonephritis or those conditions not in bold font above - (see causes of acute low back pain).
History
The history should aim to gather pertinent information to aid your diagnosis and guide management addressing the following key areas:
- Red flag symptoms (see above).
- Precipitating factor assessment (e.g. manual labour, heavy lifting, sudden movements etc.).
- Pain assessment (see below).
- Thorough neurological assessment.
- Thorough systems review to identify non-spinal causes of back pain (e.g. urinary frequency and dysuria preceding flank pain in pyelonephritis).
- Psychosocial history:
- Alcohol and drug history
- Work related injury and work duties
- Emotional state – psychological distress such as depression, anxiety and job dissatisfaction are predictors for poorer outcomes and longer symptom duration.
- Don't forget to assess for Yellow Flags
Examination
Physical examination should further identify any red flag signs, any signs of non-spinal causes of back pain, any evidence of neurological or nerve root involvement and the severity of the symptoms.
- Red flag signs (see above).
- Fever.
- Signs of shock – tachycardia, hypotension.
- Mobility assessment:
- Gait
- Sit-to-stand, bed mobility, stairs.
- Straight leg raise testing(10)
- Moderate sensitivity and positive predictive value for diagnosing herniated intervertebral disc.
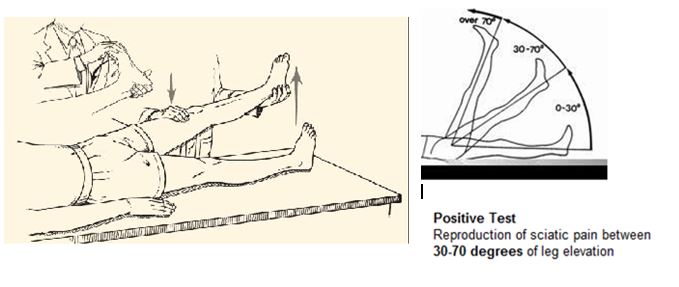
Source: http://www.rheumatologynetwork.com/articles/10-minute-examination-low-back-pain/page/0/3
- Spinal examination:
- Spinal range of motion – flexion, extension, lateral flexion and rotation
- Palpating spinous processes for local pain and exacerbation of symptoms.
- Full lower limb neurological examination including:
- Tone, power, sensation (pin prick and temperature) and reflexes
- Bladder palpation (or bladder scan) and assessing for saddle anaesthesia.
- Systems review and examination to identify non-spinal causes of back pain.
Pain Assessment
An accurate pain assessment is essential during the medical evaluation of acute low back pain and can provide vital information to assist diagnosis and guide management. Some specific considerations when assessing the patient with acute back pain are listed below:
- Severity
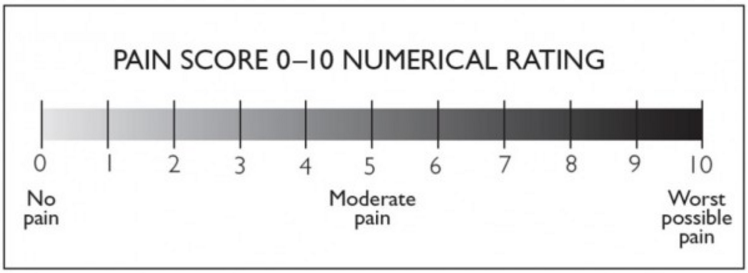
Figure - National Institute of Clinical Studies (2011) Emergency Care Pain Management Manual
Pain Score Severity
- No pain = Pain Score of 0
- Mild pain = Pain Score of 1-3 (mild distress)
- Moderate pain = Pain Score of 4-6 (moderate distress)
- Severe pain = Pain Score ≥ 7 (severe distress - red flag)
- Radiation
Back pain with radiation to either buttock or leg indicates nerve root impingement due to a herniated intervertebral disc or lumbar spinal stenosis. On occasions you may get non-dermatomal referral patterns associated with back pain and this may or may not be nerve root associated pain(9,11)
- Aggravating factors
Pseudoclaudication is the onset of leg pain during exercise or standing that is relieved by sitting or lying down in the absence of peripheral vascular disease. It is indicative of lumbar spinal stenosis.
- Duration
More serious spinal pathology is associated with pain that lasts for more than 4 weeks in duration or becomes acutely worse after a period of improvement (with appropriate management and no new aggravating factor).
Beware of the repeat ED presenters during the same episode of back pain!
- Analgesia history
Has the patient taken any analgesia?
If not – why not?!
If so – what drug, what dose, when, how often and what were the effects?
- Ankylosing spondylitis
This autoimmune condition is associated with a specific type of low back pain presentation that should alert the clinician to the diagnosis. Ankylosing spondylitis should be suspected in any patient who presents with the following symptoms so an early diagnosis can be made before the development of radiological abnormalities:
- Morning back stiffness
- Improved back pain / stiffness with exercise
- Alternating buttock pain (left and right)
- Awakening during the night due to back pain
- Younger age.
For a complete guide to emergency care acute pain management please click here.
Yellow Flags
Back to the top
Chronic Low Back Pain is defined as pain lasting >3 months (NZ ALBP Guidelines). Whilst the presence of red flags indicates the potential for serious life or limb threatening acute pathology, the presence of yellow flags indicates an increased risk of the patient having chronic back pain with resultant long term disability and work loss. It is important to identify these patients early to ensure the ED management plan can mitigate this risk where possible. This is not about extensive work-up outside the acute problem but is more about sensible and directed referral pathways. It is about reassuring this patient that the natural history of this pain is for it to get better. The pathway in a number of larger EDs is to refer these patients to in house ED Physiotherapists who have training and expertise in managing these patients. In more regional and smaller EDs this resource might not be immediately available and this may be managed in the community via the primary carer or direct referral to out of hospital local physiotherapy services.
It is not sufficient in terms of disposition to simply exclude the red flags.
- Exclude the Red Flags
- Screen for Yellow Flags in your systems work up
- Provide analgesia and directions on pain management
- Provide in hospital referral to Physiotherapy
- Provide in community referral to Physiotherapy or primary care to access that
- Consideration should also be given for referral to social work/psychologist/avoidance or caution of use of opioids or drugs of addiction for their treatment/dependence and flagging these patients to their GP and heightened importance of early motivational education for this patient population
- Provide discharge advice supported by a clear explanation of the likely benign course of the problem and set parameters for representatiion
Yellow Flag Criteria
Belief that pain and activity are harmful
Sickness behaviours
Low or negative moods, mental illness
Treatment that does not fit with best practice
Problems with compensation system
Previous history of back pain with time off work
Problems at work, poor job satisfaction
Overprotective family or lack of social support
Further information concerning the Yellow Flags can be found in the New Zealand Acute Low Back Pain Guideline.
| Spinal Causes | Non-Spinal Causes |
|---|---|
| Lumbar muscular sprain / strain | Abdominal aortic aneurysm |
| Herniated nucleus pulposis (intervertebral disc) | Pneumonia |
| Spinal stenosis / Osteoarthritis | Connective tissue disease |
| Lumbar spine fracture | Shingles |
| Degenerative disc disease | Pelvic inflammatory disease |
| Facet joint arthropathy | Prostatitis |
| Spondylosis / spondylolisthesis | Endometriosis |
Infection
| Gastrointestinal involvement
|
Congenital disease
| Renal invovlement
|
Malignancy
| Inflammatory bowel disease (cause of inflammatory arthritis) |
| Cauda equina syndrome | Psoas abscess |
| Epidural haematoma | Sickle cell disease / crisis |
| Scheuermann disease (osteochondrosis) | Sacroiliac pain / pelvic pain |
Inflammatory arthritis (often HLA-B27 associated)
| Infective endocarditis |
| Paget disease |
Source: Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Annals of Internal Medicine 2002; 137(7): 586-97.
Clinical conditions requiring urgent evaluation and senior doctor involvement are indicated in bold.
Investigations
Back to the top
Imaging
The vast majority of patients presenting to the ED with acute low back pain will require no imaging at all. Routine imaging is not indicated in patients presenting to ED with non-specific low back pain. Of the patients who require imaging only a minority require inpatient investigation with the remainder able to have imaging deferred until after a trial of analgesia and physiotherapy.
This is of particular concern when we consider that a single lumbar spine x-ray (2 views) or CT lumbar spine is equivalent to 100 and 250-500 chest x-rays respectively.
According to the RANZCR guidelines for medical imaging in acute low back pain the only recommended imaging modalities of the lumbar are x-ray and MRI, unless a vertebral fracture is the main or sole diagnosis in question (e.g. trauma) or an MRI is contra-indicated (e.g. pacemakers)
Below is an overview of the recommended imaging modalities in acute low back pain:
Urgent Imaging Recommended – Magnetic Resonance Imaging (MRI)
- Major risk factors for cancer
History of active cancer with back pain.
- Risk factors for or signs of cauda equina syndrome
Urinary retention, faecal incontinence, saddle anaesthesia.
- Risk factors for spinal infection
Fever, IVDU, recent infection, recent invasive procedure, elevated ESR, CRP or WBC, with high clinical suspicion in an at risk patient (immunocompromised, corticosteroids).
- Severe neurological deficits
Progressive motor weakness, motor deficits at multiple neurological levels.
If an MRI is contra-indicated or unavailable and the above diagnoses are suspected a CT lumbar spine may be indicated after discussion with a neurosurgeon and radiologist.
Imaging Recommended – CT Lumbar Spine
- Vertebral fracture suspected with significant trauma.
Imaging Recommended – X-ray Lumbar Spine
- Vertebral fracture suspected in:
- Osteoporotic bone (elderly, corticosteroid use) with minimal or no trauma
- Female (limit radiation).
Deferred Imaging until after a trial of therapy – MRI
- Risk factors for or signs of ankylosing spondylitis
See acute low back pain - assessment.
- Minor risk factors for cancer
Unexplained weight loss, age > 50 years, haematocrit 100.
- Risk factors or symptoms of spinal stenosis
Risk factors as listed above and patients are also a candidate for surgery.
- Signs and symptoms of radiculopathy
- Persistent back pain after 1 month of therapy
These patients will require imaging but not emergently.
No Imaging
- Previous imaging with no change in clinical status.
- No criteria for immediate imaging, less than 1 month of therapy.
RANZCR imaging decision flow chart for acute low back pain (Page 10 in below link).
For the RANZCR education module regarding current recommendations for imaging in acute low back pain please click here.
Pathology
A select group of patients will require pathology testing to assist with diagnosis and management. These requirements must be assessed on an individual patient basis.
- FBC – suspected infection, malignancy, non-spinal cause of back pain.
- ESR – suspected infection, malignancy, ankylosing spondylitis.
- Bloods cultures – febrile and suspected infection.
- Coagulation studies – neurosurgery anticipated.
- Other pathology tests including UECs, LFTs, lipase, urinalysis etc. should be considered when suspecting a non-spinal cause of back pain.
Treatment
Back to the top
Pharmacological Treatment
It is essential that a clear analgesic plan is documented in the patient notes or discharge summary, prescribed on a medication chart or discharge prescription and communicated with medical staff, nursing staff, the patient and his/her carer.
| Mild Pain | Paracetamol 1g, orally, q4-6h (Max 4g/d) | Ibuprofen1 400mg, orally q6-8h | ||
| Moderate Pain | Paracetamol 1g, orally, q4-6h (Max 4g/d) | Ibuprofen1 400mg, orally q6-8h | Consider Oxycodone2 5mg, orally, q4-6h (Max 30mg/d) | Coloxyl + Senna 2 tabs, orally, BD (with oxycodone) |
| Severe Pain | Paracetamol 1g, orally, q4-6h (Max 4g/d) | Ibuprofen1 400mg, orally q6-8h | Oxycodone2 5-10mg, orally, q4-6h (Max 30mg/d) | Coloxyl + Senna 2 tabs, orally, BD |
1 Caution with non-steroidal anti-inflammatory drug prescription in elderly (>75years), renal dysfunction, peptic ulcer disease, asthma.
Alternatively a COX-2 (cyclooxygenase 2) inhibitor may be used. Caution in patients with congestive cardiac failure in addition to the above cautions.
2 Reduce dose to Oxycodone 2.5mg, orally, q4-6h, in elderly, > 75 years
- Neuropathic Pain
Neuropathic agents are not routinely prescribed for patients with a new presentation of acute low back pain.
Consider prescribing a medication for treating neuropathic pain in those who have pain refractory to standard analgesia (> 4 weeks) or are experiencing a considerable radicular component to their pain. These patients should have had imaging done or organised and a referral pathway commenced to investigate their pain.
Start at a low dosage and increase the dose incrementally until therapeutic effect is achieved (up to the maximum dose) or unacceptable side effects prevent further use. One example is:
Gabapentin – 100-300mg, orally, nocte; increase dose gradually over 3-7 day intervals according to response; usual range 1.8-3.6g daily in 3 divided doses
- Benzodiazepines
The routine use of benzodiazepines in the management of acute back pain is not recommended. However, for a select group of patients a small dose of oral diazepam (e.g. 2.5-5mg daily) may be prescribed for the sedative effects only, in the first 24-48 hours. Be aware and tell your patients that it does not change the pain but may make them feel better about it!
- Proton Pump Inhibitors (PPI)
Consider prescribing a PPI in those patients prescribed regular NSAIDs aged > 45 years or with a history of gastro-oesophageal reflux disease.
Non-Pharmacological Treatment
Before offering non-pharmacological therapies to patients who present to ED with acute low back pain, ensure their condition and in-particular their spine is stable. Any patient presenting with red flags should receive pharmacological treatment only, until they have been reviewed by a senior doctor.
Patients who have a confirmed diagnosis of non-specific mechanical back pain and those with symptoms of back pain with radiculopathy or spinal stenosis, have been proven to benefit from early integration of non-pharmacological therapies into their management plans. Examples of such therapy modalities include:
- Encourage early mobilisation and remaining physically active
- Early physiotherapy referral
- Consideration of individually tailored structured exercise programmes
- Aerobic activity
- Movement instructions
- Muscle strengthening
- Postural control
- Stretching
- Manual therapy (not recommended in the first 48 hours)
- Spinal manipulation
- Massage
- Spinal mobilisation
- Such therapies can be performed by physiotherapists, osteopaths or chiropractors
- Consider referral for a combined physical and psychological treatment programme to those with significant pre-existing disability or psychological distress
Other Treatment Options
- Nerve Root Injection
A CT guided lumbar or sacral nerve root or facet joint injection is not routinely offered to patients who present to ED with acute low back.
Nerve root injections are offered to patients with spinal stenosis or radicular pain from a prolapsed intervertebral disc, who have persistent and significant pain, despite completing an optimal combined physical and psychological (if required) treatment programme.
A small number of patients with the above conditions may present with severe symptoms that are refractory to standard treatment. After appropriate imaging and consultation with a spinal surgeon, this small group of patients may be referred for an in-patient CT guided nerve root injection.
- Surgery
Any patient presenting with red flag signs or symptoms will almost certainly require a spinal surgical referral after senior ED doctor review. Some patients will require a more urgent referral than others, for example those with signs of cauda equina syndrome (urinary retention, faecal incontinence, saddle anaesthesia) need an urgent referral. This process will be guided by the senior doctor.
The majority of patients presenting to ED with acute low back pain will not require surgery. Referral to a spinal surgeon should be reserved for patients who still have significant pain having completed an optimal treatment programme.
Disposition
Back to the top
Admission
Any patient presenting with red flag signs or symptoms will require a hospital admission whilst appropriate investigations and management plans are implemented. Senior ED clinician review is essential to ascertain the most appropriate admission pathway. For example, if red flags are present but the senior doctor has a low index of suspicion of serious pathology, it may be appropriate to admit the patient to an ED short stay unit (EDSSU) or medical ward whilst investigations are pending. However, if there is immediate concern for significant spinal pathology, urgent spinal surgical referral with expedited investigations is imperative.
Patients presenting with acute non-specific low back or back pain with sciatica symptoms only, who fail an initial trial of therapy in the ED may require a brief hospital admission. Such failure of therapy may include ongoing pain despite adequate analgesia or poor mobility despite efforts and encouragement for early mobilisation.
The vast majority of these patients can be safely admitted to an EDSSU or medical ward and will experience sufficient symptom improvement to be discharged within the next 24 hours, if an appropriate management plan has been implemented. For the minority of patients who have ongoing symptoms negating safe discharge; re-evaluation with appropriate investigation and spinal surgery referral is required.
Discharge
Patients with no red flag criteria or those who have had serious pathology ruled out by appropriate investigations and review may be considered for discharge. Pain must be adequately controlled and they must be able to mobilise safely and independently. Social factors must also be considered including ability to climb stairs if required and necessary family or carer support.
Patient Education
Patient and carer education is paramount is ensuring successful and timely recovery. A patient factsheet should be provided. Key areas to discuss with the patient include:
- Recovery
Likely substantial recovery within 4 week with a favourable prognosis
Concerning signs and symptoms (red flags) that should prompt re-presentation
Advice regarding activities to avoid that will hinder or delay recovery
- Pharmacological Therapy
A clear explanation to the patient is required (verbally and documented). Which medications to take, how many and how often. Provide a patient factsheet to explain this.
If you assume your patient has never taken a medication before and has no previous experience managing pain you won’t go wrong!
Provide adequate prescriptions for your patient. If they present in the evening or night ensure they have an appropriate ‘take home’ pack to get them through the night.
- Non-pharmacological Therapy
Ensure physiotherapy referrals have been made or appropriate information has been provided to the patient to arrange their own physiotherapy appointment. Early mobilisation and exercise is key to their recovery.
Physiotherapy is the preferred referral process and should be encouraged, but individual preference for an osteopath or chiropractor can be accepted as an alternative.
Appropriate psychological follow-up (via the general practitioner) is encouraged when required.
- Work Cover
Ensure all relevant documentation is completed by the medical practitioner if this is a work related injury.
Discharge Letter
The discharge letter should be completed including the relevant clinical information, investigations and discharge plan specifics as stated above.
Acute Low Back Pain Patient Factsheets
Provide the patient with the above acute low back pain patient factsheet.
Follow-up
All patients who are discharged from ED after an episode of acute low back pain should follow-up with a physiotherapist (osteopath or chiropractor if the patient prefers) within the next week. However, the sooner the better, to re-enforce the exercises and strategies taught whilst in the ED.
Most patients who are discharged from ED after an episode of acute low back pain will not require medical follow-up. Exceptions to this include:
- Development of any red flag signs or symptoms – represent to the ED emergently
- Sudden deterioration in symptoms during recovery
- No improvement in symptoms despite appropriate recovery management plan
- Persistent symptoms for > 4 weeks
- Consider GP review within 4 weeks if radicular or sciatica pain is significant or not improving
- Work related injury – require a GP or specialist review within 72 hours of injury.
Cauda Equina Syndrome
Back to the top
Cauda equina syndrome is a rare but potentially devastating condition that results from the dysfunction of multiple sacral and lumbar nerve roots in the lumbar vertebral canal that can result in permanent disability (bowel, bladder and sexual dysfunction). All patients presenting to the ED with back pain must be assessed for signs and symptoms of cauda equina syndrome as clinical diagnosis is difficult with potential for considerable morbidity and associated medicolegal implications. Signs and symptoms of cauda equina syndrome mandate urgent spinal surgery referral and MRI lumbosacral spine for consideration of operative management. It is a true spinal emergency.

Source: Lavy, C. et al. Cauda equina syndrome, BMJ;2009, 338:b936
Signs and Symptoms of Cauda Equina Syndrome with Back Pain
- ‘Saddle anaesthesia’
- Reduction or loss of perianal sensation.
- Anal sphincter disturbance:
- Faecal incontinence
- Constipation
- Reduction or loss of anal tone (on PR examination).
- Urinary symptoms:
- Incomplete cauda equina syndrome.
Reduced urinary sensation, loss of desire to void, poor stream.
No urinary retention or overflow.
- Cauda equina syndrome with retention or overflow incontinence.
Incontinence at presentation is a poor prognostic sign.
Patients may present with the above signs or symptoms of cauda equina syndrome in one of three classic patterns:
- Acutely with back pain as the first symptom of lumbar disc herniation
- Chronic back pain with slow neurological progression to numbness and urinary symptoms
- The end-point of a long history of chronic back pain with or without sciatica.
Causes
- Large central lumbar disc herniation at L4/5 and L5/S1 levels.

Source: Lavy, C. et al. Cauda equina syndrome, BMJ;2009, 338:b936
- Less common causes include:
- Spinal injury with fractures or subluxation
- Spinal neoplasms – primary of metastatic
- Infective abscess or spinal osteomyelitis
- Iatrogenic – spinal anaesthesia, epidural haematoma (post-operatively), spinal manipulation.
Investigation and Management
When signs or symptoms of cauda equina syndrome are present urgent senior ED doctor review should be sought.
Urgent MRI scan is the investigation of choice. Where this is unavailable a CT scan should be performed.
Routine pre-operative blood tests and investigations (e.g. ECG) should be taken including coagulation studies and a blood group and hold. Blood cultures should be taken if febrile and there is suspicion that spinal abscess or osteomyelitis is the cause of cauda equine syndrome.
Urgent spinal surgery referral should be made without delay and prior to investigations being completed. The patient will most likely require urgent surgical decompression. The timing of surgery is somewhat controversial and will be decided upon clinical and radiological review by the spinal surgeon.