Fournier's Gangrene
Fournier’s gangrene is a type of polymicrobial necrotising fasciitis, causing a rapidly progressing infection of the genitals and perineum. Again, this is a time-critical presentation.
Fournier's is more prevalent in the older population, particularly those with co-morbidities as listed below. The male:female ratio of 10:1 is likely to reflect the better drainage of the female genitalia. It can occur in any age group. Of those occurring in the paediatric age group, two thirds are younger than 3 months. The mortality rate is close to 40% (Verma, 2012).
5 leading predisposing factors:
- Diabetes
- Hypertension
- Chronic Liver Disease
- Liver Cirrhosis
- Chronic Renal Insufficiency
The infection is usually polymicrobial, with microbes behaving synergistically resulting in rapid fascial destruction and necrosis. At least 3 organisms are cultured from each diagnosed patient. The most common organisms involved include:
- E.coli
- Bacteroides spp.
- Streptococcus spp.
- Staphylococcus.
- Enterococcus spp.
- Clostridia
- Klebsiella
- Proteus
Presentation
Pain is usually severe and out of proportion to clinical signs.
As the disease progresses, pain may subside due to necrosis of the nerves.
The patient may present in severe septic shock.
Clinical Examination
Examination of the scrotum/perineum may reveal:
- Erythema, possibly macerated or necrotic tissue in late stages
- Swelling/oedema
- Tenderness
- Subcutaneous crepitus
- Dusky appearance of skin
- Obvious gangrene
Fournier Gangrene Severity Index (FGSI) (Verma, 2012)
The FGSI is scoring system to predict the mortality of patients with fournier’s gangrene based on a combination of their physiological parameters at hospital presentation. A score of 9 or more correlates with increased mortality.
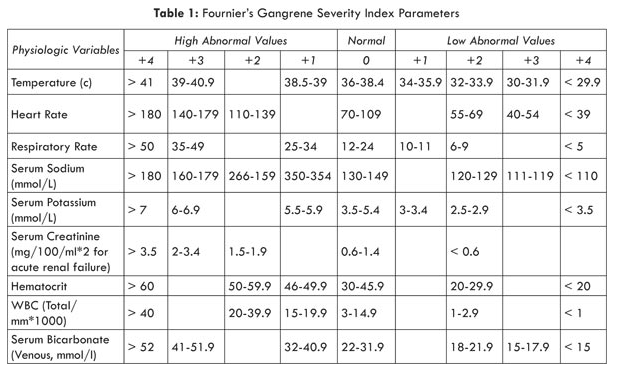
Source: https://arcuataart.files.wordpress.com/2014/03/untitled.png
Investigations
Diagnosis is based primarily on clinical findings.
- Blood tests:
- FBC, EUC
- vBG – to look for lactic acidosis as a sign of septic shock
- Coagulation profile – to assess for DIC
- Blood cultures
- Urinalysis and Urine MCS
- Wound swabs MCS
- Pelvis Radiographs/CT scan
- A surgical review should occur immediately, and if the clinical diagnosis is clear, intervention with debridement should not be delayed for imaging.
- If performed both modalities may reveal the presence of subcutaneous gas
- A CT scan may further delineate the extent of the disease process
Treatment
Immediate surgical consultation for debridement of necrotic tissue.
Broad spectrum intravenous antibiotic therapy
May require aggressive fluid resuscitation +/- vasopressor support and ICU admission.
Consider tetanus prophylaxis in these patients with soft tissue infection.
Complications
- Septic shock
- Loss of reproductive organs/impotence
- Multi-organ failure – ARDS, hepatic failure, DIC
- Death