Potassium - Hyperkalaemia
Background:
- Hyperkalaemia defined as serum K+ >5.5mEq/L
- Hyperkalaemia is potentially life threatening, and can result in cardiac arrythmias and sudden death
Causes:
MECHANISM | CAUSE |
Pseudo hyperkalaemia | Blood sample handling Haemolysis Thrombocytosis Severe leukocytosis |
Cellular potassium release | Tissue damage Rhabdomyolysis Insulin deficiency Metabolic acidosis |
Hypoaldosteronism | Primary adrenal insufficiency Pseudo hypoaldosteronism Hyporeninaemia (diabetes, interstitial kidney disease) Adrenal enzyme defect Heparin HIV |
Renal failure | Reduced potassium excretion |
Volume depletion | Reduced excretion K due to reduced sodium and water delivery to distal tubules |
Drug induced | Potassium supplements Potassium sparing diuretics ACE inhibitors Angiotensin II receptor blockers (ARBs) NSAIDs Trimethoprim Ciclosporin Pentamidine |
Other | Hyperkalaemic periodic paralysis |
Table 1. Causes of hyperkalaemia
Assessment:
History and examination:
Clinical manifestations of hyperkalaemia are uncommon with values < 6.0mmol/L.
Common acute manifestations of significant hyperkalaemia include muscle weakness or paralysis and cardiac conductions abnormalities. Physiologically, one will find a reduced urinary acid excretion resulting in a normal anion gap metabolic acidosis (due to decreased renal ammonia-genesis)
Hyperkalaemia can be initially asymptomatic or can presents with severe symptoms/signs:
Severe muscle weakness or paralysis.
- Ascending muscle weakness or paralysis that begins with the legs and progresses to the trunk and arms. Can progress to flaccid paralysis. Sphincter tone and cranial nerve function typically intact.
- Respiratory muscle weakness is rare.
Cardiovascular
- Electrocardiographic changes (as above) that may suggest the diagnosis before the blood test results.
- Conduction abnormalities (bradycardia) and arrhythmias (as above).
Management
Investigation
Any potassium abnormalities found on either a venous blood gas - or serum blood sample, should be re- confirmed on a serum sample. Do not let this delay treatment in clear cases of hyperkalaemia (consistent history, ECG changes).
In significant hyperkalaemia, an urgent ECG should be obtained to establish whether cardiotoxicity is present, and continuous ECG monitoring should occur until serum potassium values are brought into a safer range and resolution of cardiotoxicity is observed.
After confirming the diagnosis of hyperkalaemia, assessing the following is essential for optimal choice of therapy:
- Volume status: volume depletion should be corrected to ensure kidney function is optimised
- Kidney function: exclude acute kidney injury (AKI).
- ECG changes: conduction disturbances are more likely when there is a rapid risk in potassium
- Digoxin levels: in appropriate context i.e., acute, or chronic digoxin toxicity
- Check for adrenal insufficiency
- FBC: looking for normocytic, normochromic anaemia, which may suggest acute haemolysis), thrombocytosis and/or leucocytosis.
- Venous blood gas: looking for metabolic acidosis and a comparable potassium level.
- Glucose
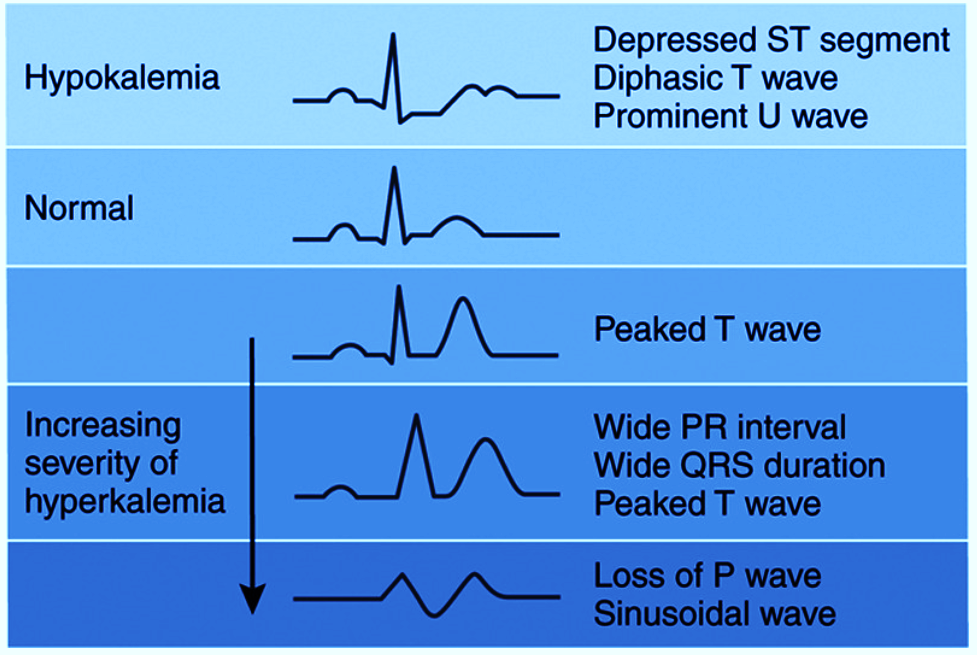
ECG Findings
Several characteristic electrocardiogram (ECG) abnormalities associated with hyperkalaemia exist, such as:
- Tall, peaked T waves and shortened QT intervals (earliest waveform changes).
- Progressive lengthening of the PR interval and QRS duration.
- Loss of the P wave morphology with progressive lengthening of the QRS interval into a sine wave.
The above ECG changes can progress to life-threatening arrhythmias including, and not limited to:
- bradycardia, sinus arrest, slow idioventricular rhythms
- ventricular tachycardia, ventricular fibrillation
- asystole with ventricular standstill - a flat line – showing complete absence of electrical activity.
K+ (mmol) | ECG changes |
5.5 – 6.5 | Peaked T waves |
6.5 – 7.5 | Flattening then loss P wave |
>7.5 | Widening QRS |
>8.0 | Sine wave, VT, VF |
Treatment
Emergency treatment for life-threatening hyperkalaemia is:
- Calcium gluconate (stabilise myocardium, not lower serum K)
- Salbutamol (temporising measure, not definitive)
- Correct any volume depletion (optimise kidney function)
- metabolic acidosis is present, intravenous bicarbonate
- Insulin and glucose
- Monitor for hypoglycaemia and correct as necessary
- Removing potassium from bowel (less urgent, slower acting)
- Dialysis (in severe cases, none of above approaches may be effective)
- Medication review
- Seek and treat cause
Specific cases:
- Primary adrenal insufficiency/hypoaldosteronism - give hydrocortisone and NOT insulin
- Digoxin toxicity - use of digoxin immune Fab (digibind) if severe life threatening arrythmia or severe ECG changes due to hyperkalaemia, use treatment as below.
TREATMENT
| DOSING |
Calcium gluconate
| Calcium gluconate 10% 10 mL IV over 2-3 mins into a large vein May need repeat 30-60min |
Salbutamol | Salbutamol 10mg via intermittent nebulisation |
Correct any volume depletion (a) No acid-base disturbance
(b) Metabolic acidosis present | (a) N. Saline iv – titrate to level depletion (b) Sodium bicarbonate 8.4%, 50 mL IV over 5-10 min |
Insulin and glucose (a) Standard therapy | (a) Short-acting insulin 10 units IV bolus PLUS Glucose 50% 50 mL IV over 5 min OR Glucose 10% 250 mL IV over 15 min (if 50% causing vascular irritation) (b) Glucose 10% IV infusion at 75 to 100 mL/hour *rule out hypoglycaemia prior commencing treatment. Monitor and treat for hypoglycaemia every 30mins for 2hrs, then hourly for 4hrs. |
**Remove Potassium from bowel
| Sodium polystyrene sulfonate 15 g PO, TDS OR 30g PR OD OR Calcium polystyrene sulfonate 15 g PO TDS OR 30g PR OD |
Dialysis | If none of above approaches effective |
Medication review | Stop drugs causing hyperkalaemia – see table 1. |
**Gastrointestinal cation exchangers - use contentious in patients not requiring dialysis. Discuss with inpatient team prior to administration
Consider consultation with critical care team:
- Severe hyperkalaemia
- Requiring dialysis