Published: July 2023
The Far West Local Health District (FWLHD) specialist palliative care service provides 24-hour support to people living with a life-limiting illness and their families, whether at home, in hospital or aged care. Specialist palliative care teams are based in Broken Hill and Buronga and provide regular face-to-face and virtual care appointments to communities across the Far West. The service partners with other healthcare professionals across the district to ensure that people can access palliative care support when and where they need it. Palliative care services can be provided by:
- palliative care nurses
- palliative care doctors
- Aboriginal health workers
- allied health providers such as dieticians, occupational therapists, physiotherapists, social workers and bereavement counsellors
- volunteers.
No referral is required to access most palliative care services; however, a doctor's referral is required to see a palliative care doctor.
24/7 support for people with life-limiting illness
Care delivered in inpatient, outpatient, community, home and RACF care settings
Multidisciplinary teams
Needs based approach for patients with life limiting disease in the last year of life
After hours support
Needs-based approach
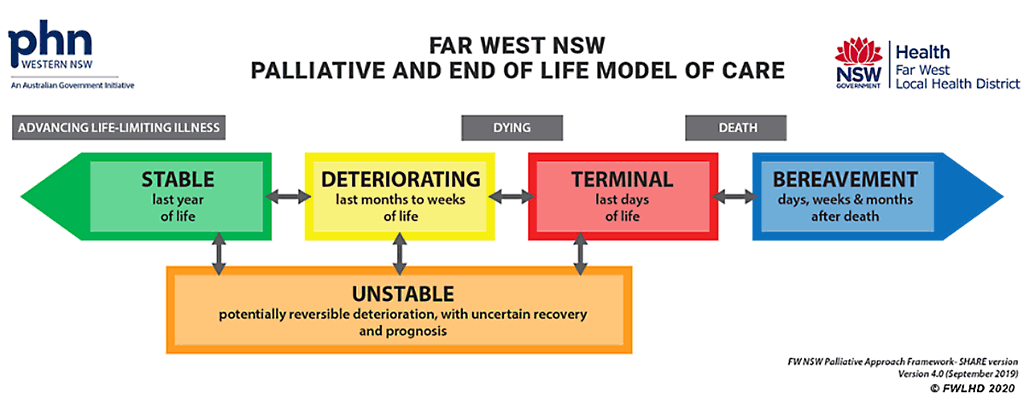
The FWLHD palliative and end of life model of care is an individualised, yet standardised, needs-based approach for the care of patients with life-limiting disease in the last year of life. The model has been translated into an electronic resource, known as electronic Palliative Approach Framework (ePAF). ePAF aims to assist carers and healthcare professionals to assess, plan and care for patients with advancing life-limiting illness.
The model is both adaptable and inclusive, which makes it relevant and applicable to various health settings and medical conditions. The embedding of the model into practice enables the specialist palliative care service to support complex cases while supporting generalist providers adopt a palliative approach to care. A practical example of this is the application of standard medication guidelines. The adoption of the guidelines has ensured patients are prescribed appropriate palliative medications as needed. This has been achieved through using established relationships with local pharmacists and general practitioners to ensure timely and pre-emptive access to palliative medications.
Benefits of using the model
Early analyses from interviews with generalist providers suggest that the model has:
- improved outcomes for patients approaching the end of their lives, as well as for their families and carers
- enhanced communication, integration and collaboration between healthcare providers within and across remote communities in Far West NSW
- increased clinicians’ knowledge, skill and confidence to provide a quality palliative approach to care
- extended the capacity of the local Specialist Palliative Care Service for more complex care and support.
Useful tips
It is important to build relationships at all levels – without them the model would not succeed.
There are three elements services should consider before implementing the model in their own local context:
- Specialist palliative care service/team structure - with clear roles and responsibilities to drive the vision, build partnerships and provide ongoing education and training
- Access to care and resources – including financial support to fund required equipment, new staff positions and training opportunities
- Strategic leadership and governance – clear direction and support from a palliative and end-of-life steering committee that aids awareness and the consistent application of the model.
Download the full local initiative for the Palliative and end of life model of care (PDF 275.0 KB).
More local initiatives
- NSW Paediatric Palliative Care Programme
- Specialist Community Palliative Care Triage Guideline
- Palliative care for patients in correctional facilities
- AMBER Care Bundle
- Delivering palliative care virtually
- HealthPathways for palliative care symptom control COORDINARE
- Extended Hours Community Palliative Care Service