Tick Bite Nurse Management Guidelines
Red Flag Exclusion Criteria
Child at risk of significant harm
Suspected non-accidental injury
Unplanned repeat ED presentation
One or more of the following (signs and symptoms of envenomation / tick paralysis / allergy / anaphylaxis)
Non-localised rash
Blurred vision
Muscle weakness
Any facial paralysis
Fever
Flu-like symptoms
Headache
Abdominal pain
Vomiting
Known allergy to tick bites (see below)
History of workplace injury
Yellow or Red Zones observations or additional criteria outlined in the NSW Health Standard Observation charts
Additional Observations
If limb affected, conduct full set of neurovascular observations
Additional History
Allergy to tick bites
Tetanus immunisation status
Management Principles
If the patient has a history of allergic reactions to tick bites, seek medical support. In these individuals ticks should be removed as soon as possible, but only by a doctor and where resuscitation facilities are readily available.
Otherwise, remove tick if still present – see below. Manual removal of ticks by forceps is the only method recommended by NSW Health.
Tick Removal
Using fine tipped tweezers or forceps, grasp tick as close to the patient’s skin as possible.
Using a smooth, steady upward motion pull tick straight out of skin (don’t bend or twist while removing)
Avoid other methods of removal such as methylated spirits or using heat to make the tick detach from the skin.
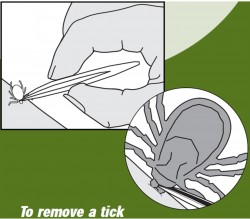
Figure 1- NSW Ministry of Health Tick Alert
Note: the favoured sites for ticks are behind ears, back of head, groin, axilla and back of knees
After removal, clean area where tick was located with appropriate antiseptic solution.
Cold compress can be applied to reduce pain and swelling
Administer analgesia as per Pain (any cause) NMG if required
Provide patient with Tick Discharge Information Sheet
Advise patient to seek immediate medical advice if severe pain, headache, fever, aching joints, abdominal pain and / or vomiting develops
References / Further Resources
Australian Resuscitation Council (2012). Guideline 9.4.3 Envenomation - Tick Bites and Bee, Wasp and Ant Stings Australian Resuscitation Council, Melbourne
Centers for Disease Control and Prevention (2012) Ticks Centers for Disease Control and Prevention, Atlanta
Needham, G.R. (1985) Evaluation of five popular methods for tick removal Pediatrics 75(6):997-1002
Department of Health (2015) Tick bite prevention Factsheet Australian Government Department of Heatlh, Canberra
NSW Ministry of Health (2013) Ticks NSW Ministry of Health, Sydney
Pitches, D.W. (2006) Removal of ticks: a review of the literature Euro Surveill 11(33)