The 10 Building Blocks of High Performing Primary Care
As a conceptual model, The 10 building blocks of high-performing primary care (1) identifies and describes the essential elements of primary care to facilitate high performance.
The model was developed using site visits, the experiences of practice facilitators, a review of existing models, and research on primary healthcare improvement and practice transformation. It is underpinned by existing frameworks for understanding the key attributes of high-performing primary care, and recognises and addresses some of their limitations. These frameworks include:
- Starfield’s four pillars of primary care(2)
- Joint principles of the Patient-Centred Medical Home (PCMH)
- Patient centred medical home recognition standards.
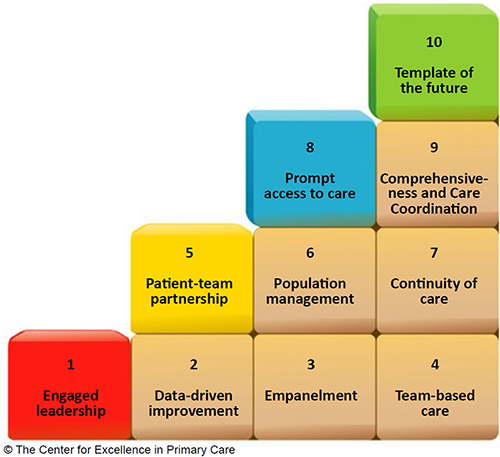
The 10 building blocks of high-performing primary care. (1) Reproduced with the permission of the author.
The building blocks include four foundational elements: engaged leadership, data-driven improvement, empanelment (patient registration), and team-based care. These foundational elements support the implementation of the other six building blocks: patient-team partnership, population management, continuity of care, prompt access to care, comprehensiveness and care coordination, and a template of the future.
Block 1 - engaged leadership: This element creates a practice-wide vision with concrete goals and objectives. Leaders are fully engaged in the process of change. High-performing practices have leadership at all levels of the organisation, and some engage patients in leadership roles. Leaders create concrete, measureable goals and objectives.
Block 2 - data-driven improvement: Using computer-based technology, data systems track clinical, operational and patient experience metrics to monitor progress towards goals and objectives. Performance measures are often set for clinicians and care teams within the primary care practice (by the practice). These are shared across organisational staff to stimulate and evaluate improvement. Data charts can be displayed in the practice and discussed at team meetings.
Block 3 - empanelment (patient registration): This element links each patient to a care team and primary care clinician. Registration enables the practice to calculate panel (caseload) size. (This calculation determines whether each clinician and team can reasonably balance patients’ demand for care with their capacity to provide that care.) Once panel size is known, practices can adjust workload among clinicians and teams.
Block 4 - team-based care: Practices often organise their teams into 'teamlets', pairing a clinician and clinical assistant who work together and share responsibility for the health of their panel. Practices co-locate clinicians and non-clinical staff in common work areas.
Block 5 - the patient-team partnership: This partnership recognises expertise the patient brings, as well as the evidence base and judgement of the clinician and their team. Patients are engaged in shared decision-making.
Block 6 - population management: Practices stratify the needs of their panels, and design team roles to match these needs. Three population-based functions provide major opportunities for sharing the care: caseload (panel) management, health coaching, and complex care management. In caseload management, a staff member periodically checks the practice registry to identify patients due for routine services. Health coaching is used to assess patients’ knowledge and motivation, provide information and skills, and engage patients in behaviour-changing action plans known to improve outcomes. Complex care management acknowledges that some patients often use high-cost services; it addresses the fact that patient needs are medically and psychosocially complex.
Block 7 - continuity of care: This element is associated with improved preventative and chronic care, greater patient and clinician experience, and lower costs. It requires patient registration to be in place. Reception staff are involved, to encourage patients to see the clinician they are registered with.
Block 8 - prompt access to care: Practices measure and control caseload size and build capacity-enhancing teams. Access and continuity may be in tension, and patients have a role in deciding what the priority is for a consultation.
Block 9 - comprehensiveness and care coordination: When patients’ needs exceed the practice’s capacity, the practice must coordinate care with other members of the Healthcare Neighbourhood. Practices include a care coordinator whose sole responsibility is to fulfil this role.
Block 10 - template of the future: Payment reform is required to support comprehensive patient care (including indirect care and face-to-face contact). Non-visit-based care coordination and pay-for-performance dollars can support new models of patient encounters. A more transformative funding model for primary care is a risk-adjusted comprehensive fee per patient, with adjustments for quality and patient experience. Other incentives could include sharing of health system cost savings for reductions in emergency presentations and hospital costs.
References
- Bodenheimer T, Ghorob A, Willard-Grace R et al. The 10 building blocks of high-performing primary care. Annals of Family Medicine 2014; 12(2):166-171.
- Starfield B. Primary care: Balancing health needs, services, and technology. New York: Oxford University Press; 1998.


