What is the Patient Centred Medical Home Model?
The Patient Centred Medical Home (PCMH) model encapsulates an approach to healthcare delivery that is:
- patient-centred
- accessible
- comprehensive
- coordinated
- continuous
- committed to quality and safety.
The patient centred medical home is at the heart of an integrated health system that wraps around the patient using the above features. In Australia, this medical home is typically a general practice or Aboriginal health service.
A team-based approach is used to fulfil the individual's required care. Team members include the patient and general practitioner (GP). Depending on the practice and the patient's needs, the team may also include practice administration staff, practice nurses, and allied healthcare providers such as physiotherapists, podiatrists, dieticians, diabetes educators and psychologists.
Sometimes a patient requires care from other services, such as community nursing, specialists, a hospital, non-government support organisations or social care services. These services form part of the healthcare neighbourhood. The patient and the medical home remain at the centre of this healthcare neighbourhood. In accordance with the principle of coordinated care, the neighbourhood supports the medical home and remains connected with it.
The healthcare neighbourhood seeks to build and support care, to be as close to the patient as possible. Specialist and hospital services play a role to strengthen the capacity of community-based services, so they may adequately support the patient. Community-based referral services assist the PCMH to support the patient and carer. The PCMH supports the wellbeing of both patient and carer. All services have a role in delivering patient care, educating for patient self-care, and helping the patient centred medical home perform its role.
To operate as one integrated health system, each service-provider group assumes an enabling role, helping other providers deliver their roles as well as possible. For example, a provider would ensure correct health information about a patient is available at the right time, and contribute to team-based care across organisations and settings.
The makeup of the PCMH and the healthcare neighbourhood depend on the roles or services needed or available in a geographic area. For example, a PCMH in one location may have just one GP and a receptionist or practice manager. Yet this PCMH may still facilitate team-based care, by linking to various services within the community through strong working relationships. The PCMH may have a small number of patients, and the capacity to provide comprehensive and coordinated care.
Another variety of PCMH is the large general practice clinic with many GPs, numerous clerical staff, an appointed care coordinator, multiple practice nurses, a full-time data manager, and a co-located psychologist, exercise physiologist, dietician, physiotherapist and clinical pharmacist. All these people are part of the PCMH and they champion its principles.
Many general practices and Aboriginal health services already exercise PCMH principles. Healthcare neighbourhoods that work with medical homes are particularly apparent in rural and regional settings. They often use formalised agreements across service providers to build good working relationships. For example, in some regional towns a number of general practices and pharmacies work on rotating shifts to provide after-hours consultations and medication.
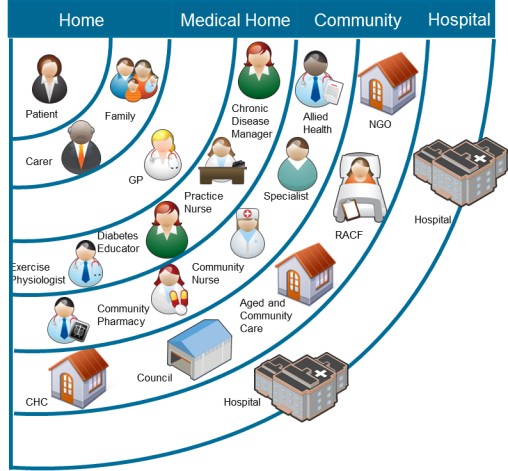
Image used with permission of Dr Tony Lembke, General Practitioner.


