The patient-reported measures strategic framework

The NSW Health PRMs Strategic Framework was developed to align existing initiatives and platforms, so that PRMs can be used across the system to enable patients to have greater input into their care.
The framework outlines the following guiding principles for the PRMs Program:
- Patient-centred: PRMs and associated processes are patient-centred and give patients a greater say in their care.
- Iterative co-design approach: PRMs are designed with input from patients, carers, clinicians and decision makers.
- Integrated: PRMs cover the patient journey across all care settings and are integrated to allow a holistic view.
- Fit-for-purpose and meaningful: PRMs need to be valued and useful for diverse groups of patients, carers, clinicians and decision makers.
- Trusted and reputable: The tools are evidence-based, culturally appropriate and easily understood.
- Consistent: The information collected and the systems used allow for comparisons across dimensions of care (core functionality, symptoms and quality of life), and allow flexibility for tailoring to local needs.
- Universal coverage: PRMs are universal but have adequate variation to distinguish between cohorts.
- Sustainable: PRMs support a sustainable health system that delivers effective and efficient care into the future.
- Transparent: Data are available in real time and accessible at multiple levels of the health system.
- Staged implementation approach: Supports the incremental adoption of PRMs and ensures adequate change management and resourcing.
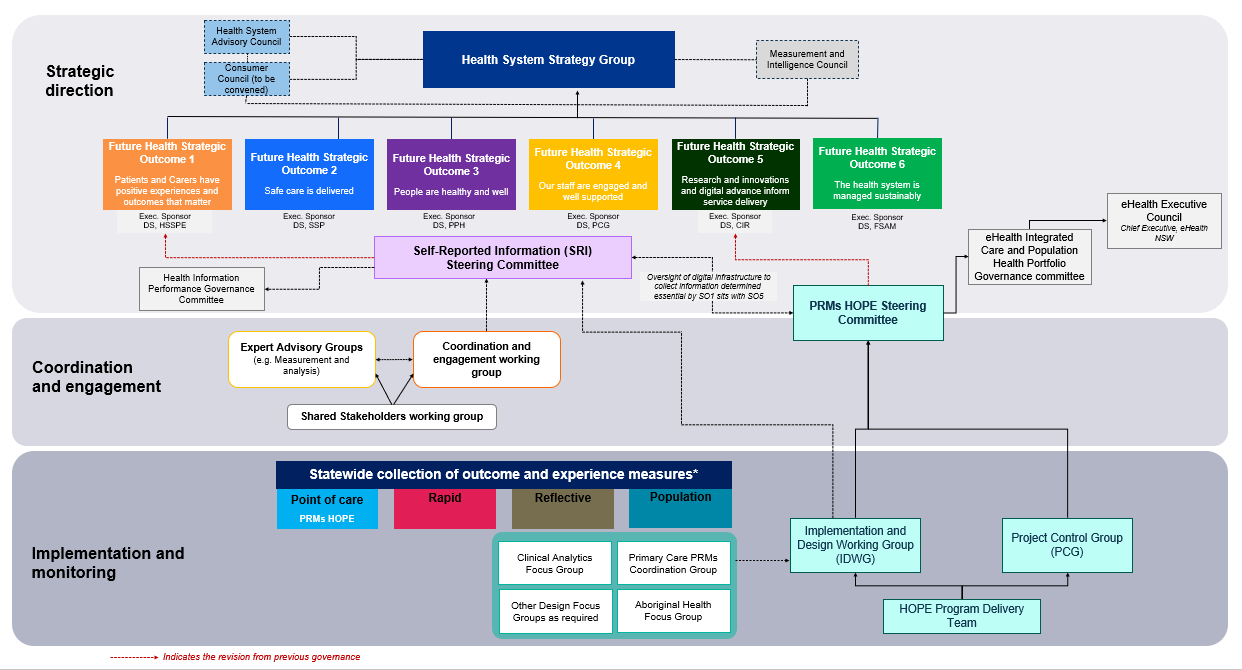
Program governance
The PRMs program governance structure is outlined in the diagram below.
Functions of the governance groups
The responsibilities of the governance groups that oversee the PRMs Program are to:
- endorse the PRMs tools, data elements, definitions and protocols (clinical and non-clinical) to be used in the statewide PRMs data collection, enabling appropriate use at the individual, service and system level
- ensure that the views of key stakeholders across the NSW health system and primary care, including priority patient populations and cultural groups, appropriately inform the choice of PRMs tools and methods of collection
- ensure the Health Outcomes and Patient Experience (HOPE) platform effectively meets and understands the technical implications of different tools and processes to meet the strategic goals of the program
- provide guidance on the implementation of the HOPE platform, ensuring it is suitable for use across the supported clinical contexts and care settings in the health system
- advise on the education, training and change management approach to support the successful adoption of the the HOPE platform across the health system
- advise on the education, training and change management approaches to support the use of effective use of PRMs in clinical practice.
- report on progress of the HOPE platform phases of development, including: milestones, risks and issues, budget allocation, monitoring of business benefits against the benefits realisation framework, quality assurance and audit, and overall performance
- provide advice on issues related to the statewide collection and use of PRMs data, to ensure this aligns with the NSW Health PRMs Strategic Framework.
Data governance and management framework
The framework outlines the principles and arrangements for the NSW health system to ensure effective management and governance of the PRM data held by the HOPE system. It defines the processes that acquire, control, protect, deliver and enhance the value of PRM data.
Download the PRMs Data Governance and Management Framework (PDF 2.0 MB)
Capability development framework
The framework describes the capabilities required of a workforce that delivers outcomes that matter to patients and carers, through collection and use of PRMs at the point of care, enabled by the HOPE platform. It is applicable for a broad range of stakeholders across healthcare settings in NSW.
Download the Capability development Framework (PDF 384.7 KB)
Change and adoption strategy
This strategy outlines the required implementation planning and support needed to shift people’s behaviours, putting into practice the desired change of collecting and using PRMs in clinical care (at point of care) and shared decision making.
Downlad the Change and adoption strategy (PDF 1.1 MB)
Stakeholder engagement and communications framework
This framework outlines the key stakeholders of the NSW PRMs Program and details the ways the NSW PRMs Program team communicates with them.
Downlad the Stakeholder engagement and communications framework (PDF 421.1 KB)