Northern NSW Integrated Care Collaborative
Introduction
The purpose of the Northern NSW Integrated Care Collaborative (ICC) was to improve care for patients with chronic and complex needs in the Tweed/Richmond network. The Collaborative was a partnership between the North Coast Primary Health Network (PHN), Northern NSW Local Health District (LHD), the Northern NSW Aboriginal Medical Services (AMS) and NSW Ambulance. Funded under NSW Health’s Integrated Care Strategy, the Collaborative was implemented from September 2015 to June 2016 as part of the LHD’s Integrated Care Program.
The ICC focused on improving health outcomes and preventing avoidable hospital admissions with the following aims:
- 200 or more patients with complex care needs managed by an Integrated Care team
- A 20% improvement in patients’ Quality of Life at nine month mark
- A 20% improvement in clinicians’ perceived connectedness of the system at nine month mark.
Project overview
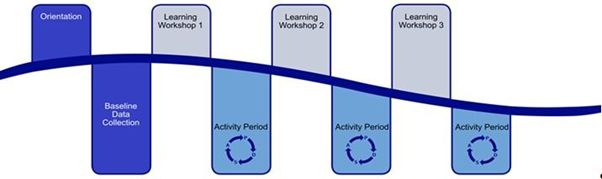
Clinicians and staff from more than twenty four acute and primary health care services participated in the ICC. Their participation involved attendance at a series of learning workshops interspersed with activity periods. During the activity periods, participants applied the workshop learnings locally. The Model for Improvement (MFI) framework was used to identify and test change ideas for making improvements in participants’ organisations.
‘Change Principles’ were selected by an expert group to guide the work of the ICC participants:
- Foundation Change Principle: Build and maintain your team
- Change Principle 1: Identify your complex cohort
- Change Principle 2: Improve your own systems
- Change Principle 3: Work as a team member
- Change Principle 4: Improve patient self-management
- Change Principle 5: Improve the wider system
Results
A total of 266 MFI cycles were submitted by forty eight participants from twenty one organisations over the eight month period of active participation in the ICC. The majority of MFI cycles, 189 (71% of the total), were submitted by the fifteen participating primary health care services. The remaining 77 (29% of the total) were submitted by clinicians and staff from the seven participating hospitals, a number of community health centres and the LHD. Most of the MFI cycles related to the building of relationships between health care providers working in different areas of the health care sector.
A total of 205 patients were enrolled in the ICC. The proportion of patients with current care plans increased from 44% to 66%. Patients with Advanced Care Directives increased from 6% to 22% and at the conclusion of the ICC, almost 17% had Shared Health Summaries uploaded to the My Health Record. During the ICC, data was collected from 82 patients about their experience of integrated care. A large majority (91%) of this group agreed that their care was well coordinated and that they and their carers were actively involved in decision making on their care and treatment (90%).
Examples of Successful MFI Cycles
This is a small sample of the changes that were developed and trialled using the ‘Model for Improvement’ cycles between the learning workshops.
Example One: Goonellabah Medical Centre
- Hosted multidisciplinary meetings with clinicians/providers from Emergency Department, perioperative administration staff, allied health and the Liver Clinic.
Example Two: Alstonville Clinic
- Recorded the number of allied health visits undertaken by patients enrolled in the ICC to enhance multidisciplinary care.
- Enhanced patient self-management by collectively determining patient goals and addressing barriers.
Example Three: King Street Medical Centre
- Developed a community health directory of services/ staff that were available for patient referrals and shared this with all interested general practices/health services.
Example Four: The Tweed Hospital
- Prior to discharge, patients were provided with a medication profile to share with their GPs at the next consultation so that current medication changes could be actioned by GPs in a timely manner. In addition, patients gained insight into the medications they were now prescribed and the reason(s) for taking them.
Benefits of the Collaborative
- Relationships between clinicians were strengthened during the ICC.
- The development of relationships provided a good foundation for the implementation of other initiatives (such as a shared care planning platform).
- Patients reported that they felt their care was well coordinated and that they were involved in their care.
- Communication between participating services improved during the ICC.
- The ICC gave rise to additional projects that will link GPs and LHDs to improve care beyond the chronic and complex patient cohort.
Challenges of the Collaborative
- The collaborative was conducted across two geographical areas. All three learning workshops were conducted at two different locations (six in total), to meet the needs of the attendees.
- Finding a convenient time for learning workshops was a challenge. Some organisations preferred to meet on weekends. The best attendances were achieved by holding shortened learning sessions after hours (5pm - 8.30pm)
- Technical and system issues delayed / precluded data collection.
Enablers for the Collaborative
- Northern NSW LHD is a NSW Integrated Care Strategy Innovator site, which allowed the LHD to fund the Improvement Foundation to manage the Collaborative.
- The LHD has a commitment to Integrated Care and provided consistent executive support for the ICC.
- The relationship between the PHN and the LHD was established and positive.
- Staff from both the PHN and the LHD supported the Collaborative, in addition to a Senior Project Manager from the Improvement Foundation.
Reflections on the Collaborative
- Nine months was a little too short for this type of collaborative. Twelve months would have been preferable.
- It would have been better to take some additional time to prepare for the collaborative before it commenced, and educate people in the Collaborative methodology first.
- Roles and responsibilities of the various organisations in supporting the collaborative need to be scoped and clarified.
- Active assistance from ICC support teams will help maintain and encourage ongoing activity and momentum.
Case study created with the kind assistance of Northern NSW LHD Integrated Care Manager, Catriona Wilson - catriona.wilson@ncahs.health.nsw.gov.au


