This project is focused on improving the outcomes of people who attend the high risk foot services (HRFS) in South Eastern Sydney Local Health District. It is an approach that improves resourcing, service access and availability of data that is relevant to staff and patient outcomes.
View a poster from the Centre for Healthcare Redesign graduation December 2021.
Aim
- Deliver a quality high risk foot service to patients with foot ulceration that meets their needs and optimises their outcomes by December 2022.
- Increase the proportion of patients attending a South Eastern Sydney Local Health District HRFS who achieve wound healing at 20 weeks by Dec 2022.
- Reduce the quarterly number of foot ulcer-related lower limb amputations from an average of 26.75 to 20 by December 2022.
- Increase the percentage of podiatrists who report as being confident and skilled in the use of the Patient-Reported Outcomes Measurement Information System (PROMIS-29) from 13% to 90% by Dec 2021.
Benefits
- Reduction in amputation rates due to foot ulcers.
- Reduction in hospitalisation and emergency department presentations due to foot ulcers.
- Reduction in unplanned admissions due to foot ulcers.
- Improved patient experience of attending HRFS.
- Improved podiatrist’s confidence and skills in collecting and applying patient reported measures.
- Improved time to healing for patients with foot ulcers.
- Increased HRFS efficiency.
- Increased local awareness of the HRFS in the community.
Background
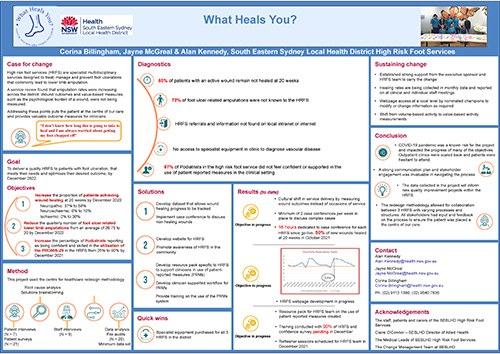
HRFS are specialist multidisciplinary services to treat people with foot ulcers with an aim to prevent lower limb amputation. In South Eastern Sydney Local Health District, annual amputation rates due to foot ulcers have doubled since 2010. Only 28% of these were known to the HRFS prior to admission.
Patients
An audit of discharges of patients from the HRFS found that only 15% of patients with an active ulcer were healed at 20 weeks following ulcer management. This means that patients are enduring the psychological and physical burden of a wound for longer than necessary.
Staff
A survey reported that 87% of staff did not feel confident and supported in using and interpreting the patient reported measures (PRMs) platform. This represents a missed opportunity to improve the quality of the service provided and improve care for individual patients. The PRMs highlight the burden of having a wound and present a quantitative measure on the effect of a clinical intervention. There are no current podiatry resources to support the team.
System
Best practice standards were consulted and HRFS equipment audits were conducted. Variations in the availability of diagnostic equipment was noted between sites. This equipment is important in the early identification and management of vascular disease. Without this equipment, vascular studies and actions can take two to four weeks longer to organise and implement and can result in a longer time to wound healing and increased amputation and mortality.1
Consultation with key stakeholders identified that referral criteria and information on the HRFS was difficult to locate online. This highlighted a barrier to timely access to the appropriate care.
The HRFS in our district only had access to activity data that was volume based. Following feedback from HRFS clinicians, a shift to value-based outcomes was important to inform the quality of care and meet statewide service standards.
Implementation
Initiation
Review and analysis of statewide guidelines revealed current service gaps in the HRFS. The project team was established. Stakeholders were identified and our executive sponsor was engaged. The project case for change was developed and the steering committee was created.
Diagnostics
This phase involved:
- patient interviews and surveys
- engagement of change management team to facilitate workshops
- process mapping and issues workshop
- staff surveys
- data analysis with the NSW Health quality improvement data system (QIDS), discern reporting portal and non-admitted patient reporting
- documentation audits
- root cause analysis and prioritisation process.
Seventy-two issues were identified and the top three problems were prioritised by the steering committee.
Solutions
The development of solutions included:
- patient interviews
- brain storming workshop with HRFS clinicians
- individual consultation with engaged stakeholders
- literature review of current best practice.
Key solutions
- Make the HRFS information easily found on the SESLHD website.
- Align with a HealthPathways project.
- Develop a flagging system on the patient record to identify patient wound progress at six weeks.
- Protect time to case conference patients who are not progressing.
- Develop an education and support pack for clinicians to access when discussing quality of life and treatment goals. The psychology team collaborated on the development of the resource.
Implementation
The implementation was guided by the project aim strategy document.
- The website was updated with a planned go-live date in December 2021.
- Toe pressure machines, required for faster vascular assessment were purchased for all sites.
- Case conferences were started while the six week flagging system was in development. This allowed team engagement and feedback with the concept.
- The resource pack was developed and additional training provided by the PRMs team.
- Data to be collated was identified. This will identify patients who are not improving six weeks after their initial appointment.
Status
Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Dates
- Start: Feb-2021
- End of pilot: Dec-2022
Implementation sites
- Prince of Wales Hospital High Risk Foot Service
- St George Hospital High Risk Foot Service
- Sutherland Hospital High Risk Foot Service
Partnerships
- Centre for Healthcare Redesign
- Central and Eastern Sydney Primary Health Network
- Agency for Clinical Innovation
Evaluation
The results of this project include the collection and evaluation of the following information.
- Wound healing rates at 20 weeks. This is currently under regular review with the team.
- Quarterly district amputation rates. This is monitored by the team every quarter and has been achieving the objective in 2021.
- Surveys where staff self-report their confidence using PROMIS-29
- Staff interaction with the PRMs platform. The use of the PRMs platform is still being integrated into usual care at all sites.
Lessons learnt
- Even across the same health district, the context at each site is different and needs to be adjusted to suit each location. Each hospital has different specialists and associated services which require different solutions.
- There is value in a generic framework, as opposed to a direct model, that has to be implemented absolutely.
- Fully assess the problem prior to reaching a solution, rather than starting with a possible solution.
- Engage the implementation leads and change managers. Engaging skilled facilitators to run workshops (external to the direct team) who can keep the entire team involved.
- You can’t plan around or prepare for a pandemic.
References
1. Prompers L, Schaper N, Apelqvist J, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia 2008 May;51(5):747-55. DOI: 10.1007/s00125-008-0940-0
Further reading
- Diabetes Feet Australia
- International Working Group on the Diabetic Foot
- NSW Agency for Clinical Innovation. Leading Better Value Care: Diabetes high risk foot services. Sydney: ACI; 2021 [updated 2021 Jul 12].
- Health Stats NSW. Amputations due to diabetes. Sydney: NSW Ministry of Health [updated 2020 Mar 24].
Contact
Alan Kennedy
Podiatry Advisor
South Eastern Sydney Local Health District
Alan.kennedy@health.nsw.gov.au
(02) 9113 1380 | (02) 9540 7836