Murrumbidgee Local Health District (MLHD) developed a process to ensure all patients have a best possible medication history (BPMH) recorded on admission to hospital.
View a poster from the Centre for Healthcare Redesign graduation, December 2017.
Aim
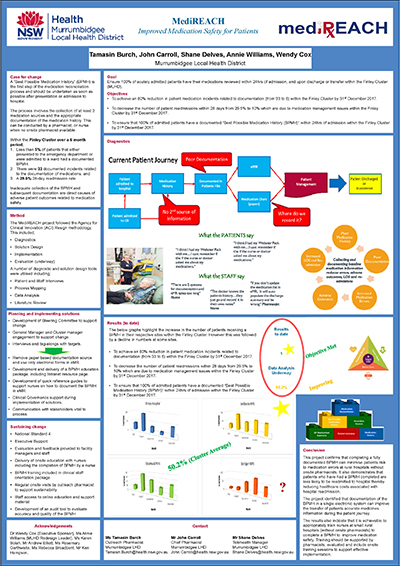
To ensure 100 per cent of acute patients have their medications reviewed within 24 hours of admission to hospitals in the MLHD Finley Cluster, by December 2017.
Benefits
- Increases the accuracy of patient medications at the time of hospital admission.
- Reduces medication errors such as omitted orders or incorrect doses on admission to hospital.
- Reduces the time spent fixing medication errors after the patient is admitted to hospital.
- Helps nursing staff understand generic medication names and formulations.
- Improves the continuity of patient care from the hospital into the community.
- Reduces costs associated with an increased length of stay or readmission to hospital, due to medication errors.
Background
A BPMH is part of the medication reconciliation process and involves interviewing the patient and their family or carer, to get an accurate and complete understanding of what medications they are taking, as well as how much and how often they are taking them. The clinician must verify this information with at least one other source to ensure it is correct, and document the results appropriately.
A BPMH should be undertaken as soon as possible after presentation or admission to hospital. The sooner a BPMH is undertaken, the less risk there is that medication errors or omissions will occur. Inadequate collection and documentation of a BPMH can reduce patient safety and lead to negative health outcomes.
An audit conducted between July and December 2016 showed that less than five per cent of patients who presented to the emergency department or were admitted to a ward in the Finley Cluster had a documented BPMH. During this period, there were 33 incidents related to medication documentation errors and a 28-day readmission rate of 29.8 per cent related to medication management issues.
Patient and staff interviews conducted between May and August 2017 showed there was a lack of understanding about medication safety processes, with some staff unclear about whose responsibility it was to collect and document a BPMH. In addition, both paper and electronic records were being used to collect and document patients’ BPMH, which confused staff and resulted in poor compliance with existing processes.
Implementation
- Key stakeholders were engaged throughout the project via face-to-face meetings, teleconferences and working group meetings, to ensure objectives were met. Stakeholders included facility and cluster managers, nursing staff, pharmacy staff and patients.
- A standardised process for collecting and documenting the BPMH in the electronic medical record (eMR) was developed, providing a ‘single source of truth’ for patients’ medical information. This allowed clinical staff to access patient details from any facility in the Finley Cluster.
- A staff education package was developed for nursing staff and managers, delivered by pharmacists via face-to-face and video conferencing sessions. Video conference sessions were recorded for absent staff and used in local orientation processes. The education package included:
- examples of medication errors that may result from taking an inadequate medication history
- a definition of BPMH and how to take a BPMH, including patient and carer interviews and using a secondary source to verify the information
- an intranet link with resources on medication reconciliation and BPMH, including local, state and national training and education resources
- a quick reference guide for nursing staff on how to document a BPMH using the patient’s eMR
- a real-life scenario where nurses were required to take a BPMH with the support and guidance of the training pharmacist.
Status
- Implementation – The project is ready for implementation or is currently being implemented, piloted or tested.
Key dates
- Project start: February 2017
- Project implementation: June 2017
- Project evaluation: December 2017
Implementation sites
- Finley Health Service, MLHD
- Berrigan Health Service, MLHD
- Jerilderie Health Service, MLHD
- Tocumwal Health Service, MLHD
Partnerships
Evaluation
A full evaluation will be undertaken in December 2017 measuring the following outcomes:
- number of patients with a BPMH taken within 24 hours of admission
- number of incidents related to medication documentation
- 28-day readmission rate, related to medication management issues.
Results
Results to date show the number of patients with a BPMH collected and documented on admission improved from less than five per cent in August 2017, to 76 per cent across the four pilot sites in November 2017, with three of the four pilot sites achieving a rate of more than 90 per cent.
Lessons learnt
- Engage with clinicians early and involve them in the process.
- Appropriate sponsorship is key to successful implementation.
- Identify champions and provide them with additional support.
- Assess the organisational climate to ensure staff are not overwhelmed with change.
- Revisit the diagnostics and solution design if required.
- Frequent, scheduled communication is essential when the project team is working across different sites.
Further reading
- Australian Commission on Safety and Quality in Health Care (ACSQHC). Match up Medicines [Internet]. Sydney: ACSQHC; 2011 [cited November 2017]
- Australian Commission on Safety and Quality in Health Care (ACSQHC). National Safety and Quality Health Service Standards [Internet]. 2nd ed. Sydney: ACSQHC; 2017.
- Australian Commission on Safety and Quality in Health Care (ACSQHC). Taking a Best Possible Medication History [Internet]. Sydney: ACSQHC; 2017 [cited November 2017]..
Contacts
John Carroll
Chief Pharmacist
Murrumbidgee Local Health District
Tamasin Burch
Outreach Pharmacist
Deniliquin Health Service
Murrumbidgee Local Health District
Shane Delves
Telehealth Manager
Murrumbidgee Local Health District
Shane.Delves@health.nsw.gov.au