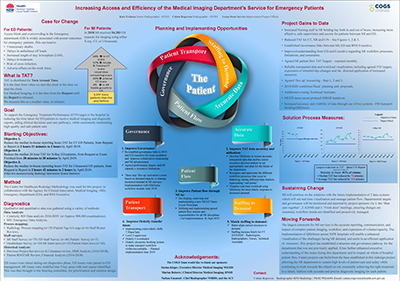
Increasing Access and Efficiency of the Medical Imaging Department’s Service for Emergency Patients
Summary
This project improves the median turnaround time for emergency department patients receiving scans at Royal North Shore Hospital.
View a poster from the Centre for Healthcare Redesign graduation, May 2019.
Aim
To improve the medical imaging department’s request to report turnaround time for emergency department patients, by achieving the following by April 2019:
- reduce the median in-house reporting hour’s turnaround time for cat scan (CT) emergency department patients, from two hours 21 minutes to two hours
- reduce the median 24 hour turnaround time for x-ray emergency department patients, from 38 minutes to 30 minutes
- reduce the median in-house reporting hours turnaround time for ultrasound emergency department patients, from 2 hours 42 mins to 2 hours.
Benefits
Benefits include:
- an improved patient experience, owing to reduced waiting times in the emergency department for examinations
- increased collaboration and improved relationships between medical imaging staff and emergency department staff
- improved staff morale in the medical imaging department
- an improvement in emergency department targets, including emergency treatment performance (ETP)
- enhanced efficiency in patient flow throughout the hospital.
Background
Access block and overcrowding in the emergency department is widely associated with poorer outcomes for emergency patients. This can lead to:
- possible avoidable deaths and complications
- increased length of stay in hospitals
- delays in ambulance off loads
- delays in treatment
- risk of cross infection
- adverse effects on the work force.
The NSW Health ETP indicator requires a patient’s total time in an emergency department to be less than four hours. This enables quicker treatment times for acute conditions and a greater access to emergency care.
Emergency treatment performance is an indicator of the whole hospital processes, as such is every departments responsibility.
In 2017, there was an 8.9% annual growth in emergency department presentations with a corresponding growth of approximately 6% in emergency department demand for imaging. This adds considerable pressure to the medical imaging department processes.
The greatest resource intensive increase has been identified as cat scans (CT). Scan requests across the hospital have experienced a year on year increase of examination numbers, with the most recent being 20% recorded for last year.
Not only does this include the approximate 6% patient increase from the emergency department, which for a single patient does not show the potential of multiple exams in multiple modalities (therefore increasing the exam load on medical imaging disproportionately to the 6% patient increase), but also the increase from wards.
N.B: The complexity of measuring turnaround time from e-order to report ready across a 24 hour period or even 0800-2400 hours is acknowledged.
Currently Royal North Shore Hospital’s ETP is 64%, compared to NSW Health’s mandated target of 75% for tertiary trauma hospitals. Patients who have not left the emergency department within four hours are considered to have breached the Emergency Treatment Performance target.
Within the four hour window the following steps are taken: clinical review, diagnosis and decision to admit or discharge the patient. These steps are required in the four hour timeframe to achieve ETP.
Imaging plays a crucial role in such decision making, when deciding the appropriate care pathway for the patient. This means medical imaging department delays can contribute to emergency department delays, which in turn can cause a patient to ‘breach’ the four hour target.
Implementation
1. Accuracy of data
This solution is to create a radiology dashboard for real time tracking and predictive capabilities, allowing the department to look at the same easy to understand information from different locations. It is important that key performance indicators are meaningful, based on objective research and interpretable both within and outside the department. This is why the project team are:
- building a Qlik app to ensure accurate data is available
- developing activity and performance measures/key performance indicators
- establishing regular medical imaging that reports to appropriate governance groups, such as the Royal North Shore Hospital executive unit, using the Qlik app.
2. Ensure medical imaging staffing matches demand for services
This solution reports on the current levels of staffing and describes the workflow by a different measure than is currently used. Currently the time the request is inputted is used to define the rosters, but this is not indicative of when the work actually hits the department.
This is why the project team are:
- better aligning current resources to demand where possible
- determining potential benefits of additional resources at peak demand times, to develop business cases where appropriate.
3a. Wards people transport process improvement
This solution ensures the workload of ward people; their journey times and peak activity are all visible and monitored. Currently there are delays in patient flow between medical imaging and the emergency department. This can cause delays in the patient’s diagnosis, treatment and admission or discharge.
This is why the project team are:
- working with HealthShare to implement and monitor the filling of extra shifts for wards people – 7am, 2 and 3pm
- implementing a Level 2 ward supervisor role for medical imaging
- creating an electronic tracking system to make transport workflow more visible and therefore, accountable.
3b. Nurse escort process improvement
This solution ensures that all patients requiring a nurse escort receive a nurse escort. This will provide safe and efficient care for our emergency department patients.
Currently there is no formalised nurse escort flowchart that medical imaging, emergency department nurses and wards people can follow.
This is why the project team are:
- creating and implementing a medical imaging and emergency department nurse escort flowchart.
4. Governance
This solution formalises key performance indicators in the medical imaging department. The goal being to measure departmental performance and create guidelines for patient flow accountability. Limited formal departmental performance key performance indicators are also reported to Royal North Shore Hospital’s operational management.
This is why the project team are:
- defining and implementing agreed patient flow actions and responsibilities for all MI disciplines
- re-establishing governance links to the Royal North Shore Hospital and emergency department leadership team - by establishing a monthly meeting
- designing a three-step activation system based on demand/capacity to better respond to increases in demand for medical imaging services.
Status
Implementation – some solutions are currently being implemented, while other long term solutions are in the early pilot stages.
Dates
- Project start date: April 2018
- Project end date: April 2019
Implementation site
Royal North Shore Hospital, Northern Sydney Local Health District
Partnerships
ACI Centre for Healthcare Redesign
Results
Since the implementation phase for all solutions is still underway, noteworthy improvements are not yet apparent. Despite this, below are some early insights and updates.
- After implementation started, the turnaround time against project objectives began to be measured. Data is being collected weekly and reflected in monthly reports.
- Once the new Qlikview app is built, then medical imaging staff and the Royal North Shore Executive will be educated on how to use the app. This will enable medical imaging to have open and transparent data.
- After ‘staffing to demand’ was mapped out during diagnostics, business cases have been written to request increased full time equivalent staff across all craft groups in medical imaging. At the time of writing it is hopeful that they can be incorporated into the budget build.
- There are some gains with the addition of extra wards people to assist with transfers to and from the emergency department. However there is still some work to do if the set targets are to be reached.
- Quantitative data is being gathered for the nurse escort flowchart, so that patients who require an escort receive an escort.
- A major issue identified in the project was the lack of agreed patient flow actions for medical imaging staff, as well as no agreed key performance indicators. Communication has been developed, and roles and responsibilities created, so staff are clear of their roles and have the capacity to meet demand when required. Meetings between medical imaging and emergency department staff have also started to help build relationships and problem solve. These will continue in order to sustain these relationships.
Implementation and evaluation will be ongoing, and improvements will continue to be made across other modalities within medical imaging and across the Royal North Shore Hospital.
Lessons Learnt
- The importance of effective communication: with many different disciplines within the medical imaging department, and multiple stakeholders, it was important to consider ‘what’s in it for them’ when communicating project details. This helped to get the correct messaging across and achieve engagement.
- The need for collaboration: the medical imaging department could not implement any solutions without the collaboration and support of the emergency department and HealthShare.
- The value of resources and time: these two factors play a huge role in any project in order for it to be successful. With the volume of work in medical imaging process and they sometimes got in the way of implementation. For example, during the diagnostics and solutions phase the project team did not expect that when implementing we would not be able to adhere to the allocated time frame. This has meant that some solutions have not progressed further at this point.
- The need for accurate data collection methods: this requires such methods to be ‘beyond scrutiny’, and it proved to be a major constraint. For example, the computer data which identified and measured each step was flawed; time stamps were open to interpretation, and complex. This gave an opportunity for information being ‘open to interpretation’, and extensive discussions on what time stamps to use are largely still unresolved. The consequence of this was that all other solutions were severely impacted as they were hard to define, measure and even prove that this was where the problems lie, giving active objectors ample reason to continue to block innovation.
- An understanding of the complexities of medical imaging at a higher executive level: these projects require a depth of communication across a broad spectrum of stakeholders and stakeholder-wide engagement and sponsorship in this area.
Contacts
Katherine Erdman
Section Senior Radiographer
Royal North Shore Hospital
Northern Sydney Local Health District
Phone: 02 9926 4400
Katherine.erdman@health.nsw.gov.au
Calum Rogerson
Radiographer
Royal North Shore Hospital
Northern Sydney Local Health District
Phone: 02 9926 4400
Calum.rogerson@health.nsw.gov.au
Lenae Dean
Service Improvement Project Officer
Royal North Shore Hospital
Northern Sydney Local Health District
Phone: 02 9463 1908
Lenae.dean@health.nsw.gov.au