Summary
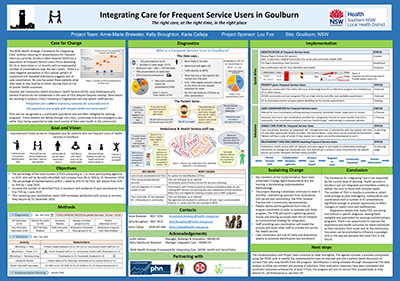
This project brings together the local ambulance service, general practice (GP), hospital emergency department (ED) and community health centre resources to identify and respond to patients who repeatedly use one or more of these health services.
These agencies will work collaboratively with the patient to provide a coordinated, targeted and timely response to the general health and social needs that the patient identifies as triggering their need for an emergency response.
View a project from the Centre for Healthcare Redesign graduation, May 2019.
Aim
- By 31 December 2019: the percentage of total frequent service users (FSUs) presenting to one or more participating agencies in 2019 will increase from 0% to 30%. These FSUs will be formally identified
- By 1 June 2020: the percentage of representations by FSUs, within one week to Goulburn Hospital ED, will reduce from 42% to 20%
- By 1 June 2020: the number of FSUs in Goulburn with evidence of care coordination will increase from 0 to 75%
- By 31 December 2020: FSUs receiving care coordination will report 50% increased satisfaction with access to services they require. The baseline is established at enrolment in care coordination.
Benefits
Benefits to the patient
- I will be identified as someone needing extra help.
- There will be one person helping me get what I need to stay healthy.
- I will be able to get the help I need when I need it.
- I will have a plan which covers all my health needs.
- Everyone who is helping me with my health will know what is going on.
Benefits to carers
- I will be included in planning care. I will know who to contact if I am unsure about arrangements.
- I will be able to ask questions and I will be listened to.
- We will have more control.
Benefits to the health service
- There will be someone to help patients sort everything out. Someone will get in touch soon after they leave hospital.
- There will be a single care plan covering many different issues.
- There will be meaningful cross agency discussion to help get care and support organised.
Benefits to ambulance
- We’ll know where to refer frequent service users. It won’t be a guess.
- We’ll know if they got the follow up care they needed.
- There will be one person we can contact.
Benefits to general practice
- I will know more about the other services my patients are attending.
- I know my patient will get seen quickly. They will be linked in to the services they need.
- I know who I can refer to in other services.
Background
An emergency department is a common touchpoint with the health service.
It is free, open 24 hours and there is always a doctor available. However it is not the ideal place to manage care for patients who have complex health and social needs beyond their reason for presentation.
In 2017, 19 patients presented to the emergency department 10 or more times, with file audits revealing no evidence of referral or care coordination. This is despite clear indication for multidisciplinary involvement and ongoing care needs.
There is a clear negative perception of FSUs whose pattern of repeated service use evidences a lack of integrated and coordinated care. Evidence shows that these patients are recognised and often well-known to the ambulance and health service staff, however there is no system to formally and consistently identify FSUs and no avenue to action a response.
Current community-based programs that provide coordinated care have age and diagnostic related group eligibility criteria. This excludes many patients who frequently use emergency departments, given more than half of this cohort are younger than the eligible age.
'Integrated care is vital to improving outcomes for vulnerable and at risk populations and people with complex health and social needs'1
Services in Goulburn are not integrated, and the capacity to provide coordinated care is limited by current models of service delivery. There is a cultural and communication divide between the emergency department, the community health centre, the GP and ambulance; each with separate systems for documentation and various points of access. Staff and services are providing great care, but working in silos. There are no forums to facilitate cross agency discussion for FSUs, and staff admit that they rarely speak with the patient’s GP. Patients, their carers and staff are not aware of who is already involved or who to contact if needed.
In summary, the current system does not provide an opportunity for staff to empower FSUs to better manage their own health. It also does not address potentially avoidable emergency department presentations or avoidable calls to the ambulance service. Health services in Goulburn are working towards providing coordinated, integrated and person-centred care in alignment with the current Strategic Framework for Integrating Care in SNSWLHD.1
Implementation
Five solutions were generated from workshops that were held with key stakeholders from ambulance, the primary health care network and the health service.
Solution 1: A system to identify frequent users of health services in Goulburn
'I will be known to health services as someone needing extra help.'
By leveraging existing electronic medical record systems, an alert will be manually assigned to a patient’s file when they present to ED more than eight times in a 12 month period. An equivalent alert will be placed with the ambulance data terminal and their GP will be notified. Reports will be generated on these patients, and a case discussion will follow (see solution 3 and 5).
Solution 2: Frequent service users are prioritised for health services in Goulburn
'I will be able to get the help I need when I need it.'
Frequent service users will receive priority appointments with their GP and also community health services, rather than possible placement on a waiting list.
Solution 3: Intensive care coordination for frequent service users
'There will be one person helping me get what I need to stay healthy.'
Once identified, an assigned care coordinator will contact the frequent service user within 48 hours of ED presentation. This role will provide intensive short term support and facilitate information sharing and shared care planning across services. A ‘health coaching’ approach will be used to empower patients in self-management and having a proactive approach to their health.
Solution 4: Integrated self-management plan that supports shared decision making
'I will have a plan which covers all my health needs.'
A single shared care plan will be developed with the patient, their carer, GP and relevant health professionals. The plan will be held by all relevant agencies, and uploaded to a patient’s My Health Record (if applicable). The patient will have a copy and the ambulance service will be alerted to this on their data terminal.
Solution 5: Patient case discussion into the agenda of current multidisciplinary team meetings
'Everyone who is helping me with my health will know what's going on.'
Patients and carers will be part of case discussions with ambulance staff, their GP, community health centre and ED (as applicable). Case discussions will be built into existing multidisciplinary forums to avoid duplication, but expanded to encompass multiple agencies.
All solutions leverage existing resources and systems in place to strengthen the sustainability of the project.
Status
Implementation - The initiative is ready for implementation, is currently being implemented, piloted or tested.
Dates
February 2018 to December 2020
An implementation working party began work on 14 March 2019. They meet fortnightly to progress the solutions, as per schedule outlined below. This team has representatives from the ambulance service, the primary health care network, ED, GP and the health service.
Members have started training in accelerating implementation methodology (AIM) and Health Change Methodology.
Solution 1: Flag in medical record
- April 2019: Start flag in ED
- July 2019: Progress above process to ambulance and GP
Solution 2: Priority appointments
- February 2019: Cross agency agreement to prioritise FSUs for appointments
- March 2019: Promotion and education across agencies
- May 2019: Service referrals start
Solution 3: Intensive care coordination
- February 2019: Identification of staff, establishment of care coordination responsibilities.
- March 2019: Training provided in care coordination and health coaching, communication and promotion with other agencies
- May 2019: Enrol patients
Solution 4: Integrated self-management plan
- March 2019: Draft integrated self-management plan
- May 2019: Publish, implement use. Continue plan-do-study-act cycle with form.
Solution 5: Patient case discussion
- Oct 2018: Review of existing multidisciplinary team forums
- March 2019: Establish forum for case discussion of potential patients to enrol, as part of the implementation team meetings
- May 2019: Once patients enrolled, coordinate community case conferencing with nominated GP
- July 2019: Progress FSU identification and case discussion into existing multidisciplinary team forums.
Implementation sites
- Goulburn Health Service
- Ambulance Service NSW Goulburn
- General Practice - Clinton Medical Centre
Partnerships
- NSW Ambulance - Goulburn Sector
- COORDINARE- South East NSW Primary Health Care Network
- Southern NSW Local Health District
- Centre for Healthcare Redesign
Evaluation
Evaluation results are not available at time of writing. First solutions will be evaluated at the end of 2019.
Lessons learnt
- Engage all project stakeholders. Particularly to understand that their ‘what’s in it for me’ is critical to project success.
- Obtain the input of patients. This is important and it can be difficult with transient and disenfranchised patient groups. The time required to engage with patients can conflict with project timeframes, so this has been built into plan-do-study-act cycles during implementation.
- Obtain ethics required to conduct patient interviews. This important step added considerable delays to project timeframes. There is ongoing debate between agencies on the differences between ‘research’ versus ‘quality projects’ in the health sector. This requires further organisational review and development.
References
- NSW Ministry of Health. NSW Health Strategic Framework for Integrating Care. Health and Social Policy. 2018
- Coordinare, South Eastern New South Wales Primary Health Network, Southern New South Wales Local Health District. Southern New South Wales integrated care strategy. 2018.
Further reading
- Olsson M, Hansagi H. Repeated use of the emergency department: qualitative study of the patient’s perspective. Emerg Med J. 2001;18:430-434.
- Daniels J, Osborn M, Davis C. Better safe than sorry? Frequent attendance in a hospital emergency department: an exploratory study. Br J Pain. 2018;12(1):10-19.
- Miller KE, Duan-Porter W, Stechuchak KM, et al. Risk stratification for return emergency department visits among high-risk patients. The American journal of managed care. 2017 Aug;23(8):e275-9.
Contacts
Anne Brewster
Physiotherapy Manager
Goulburn Health Service
Southern NSW Local Health District
Phone: 02 4827 3256
AnneMarie.Brewster@health.nsw.gov.au
Karla Calleja
Corporate Information Manager
Southern NSW Local Health District
Phone: 0436 647 669
Karla.Calleja@health.nsw.gov.au
Kelly Broughton
Clinical Nurse Specialist, Hospital in the Home
Goulburn Health Service
Southern NSW Local Health District
Phone: 0457 525 505
Kelly.Broughton@health.nsw.gov.au
Netty Swinburn Mepham
Manager Integrated Care
Ambulatory and Integrated Care
Southern NSW Local Health District
Phone: 0417 026 226
Netty.SwinburneMepham@health.nsw.gov.au