This project focuses on designing tools and resources for NSW hospitals to implement the National Surgical Quality Improvement Program (NSQIP) in their service.
View a poster from the Centre for Healthcare Redesign graduation, December 2018.
Aim
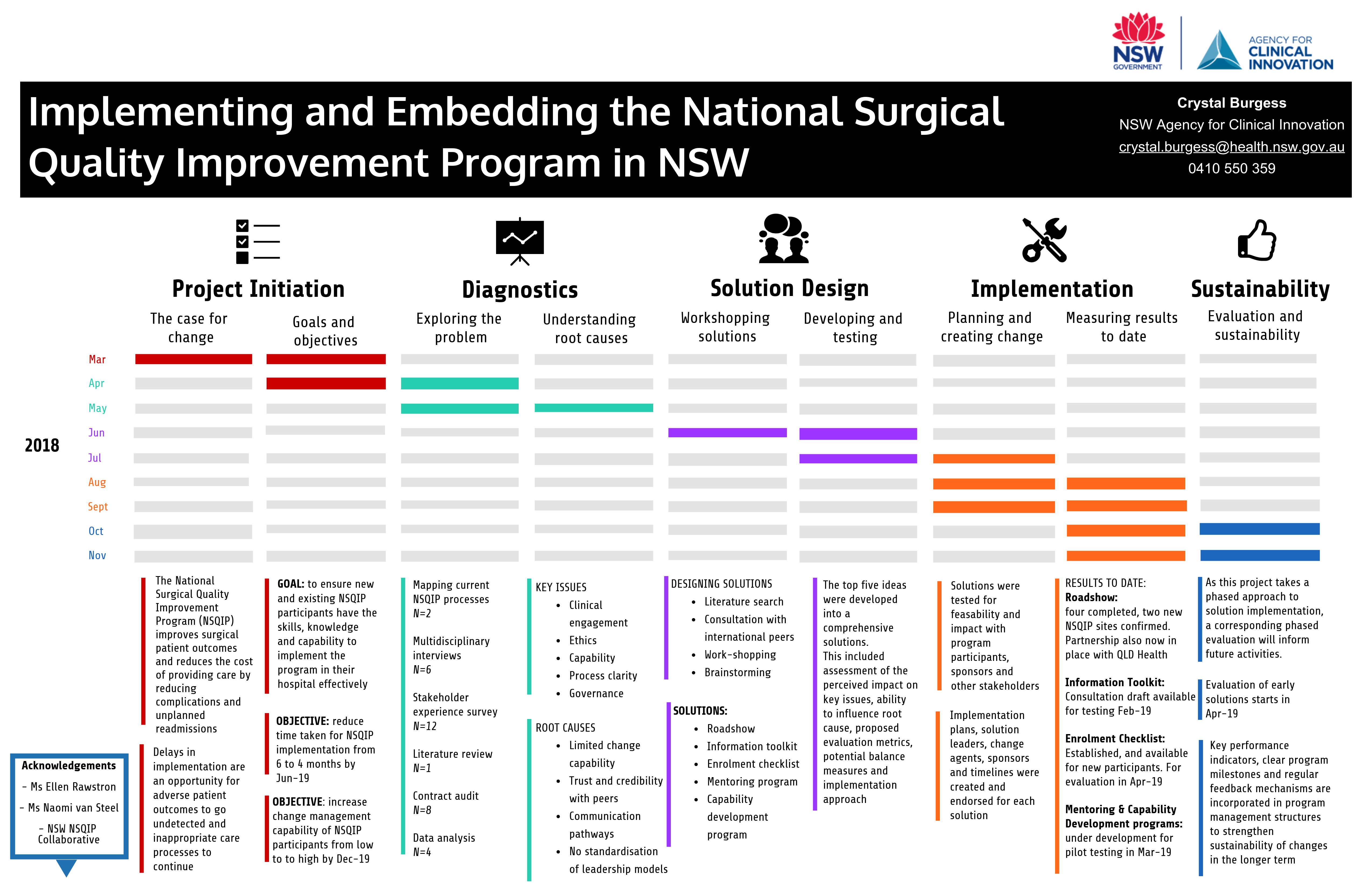
- Reduce the time between contract execution and data collection from a median of six to four months by July 2019.
- Increase program management skills and capabilities to successfully deliver NSQIP in their local environment by Dec 2019.
Benefits
This project will reduce barriers to the implementation of NSQIP in NSW by:
- fast-tracking sites to commence quality improvement initiatives
- supporting improved surgical patient outcomes
- reducing the cost of care delivery.
Background
NSQIP is a surgical quality improvement initiative that allows a hospital to identify areas for performance improvement and develop local strategies to address them. It has been shown to improve patient healthcare outcomes by reducing unplanned re-admissions, post-operative complications, and subsequent cost of care delivery.1-3.
Investigation into current processes and experiences of the NSQIP program in NSW uncovered seven root causes contributing to barriers in enrolment and implementation. This has resulted in lost opportunities to improve the quality and safety of patient care, potentially allowing additional adverse events to occur.
Furthermore, delays to enrolment and implementation erode the enthusiasm and confidence of program participants. Failure to embed the program within the surgical service in a timely manner, communicate effectively with stakeholders and take action from performance results, limits the viability of the program and puts long term sustainability at risk.
Implementation
To address these barriers, five solutions have been designed to increase clarity of enrolment processes, better articulate roles and responsibilities within the program, increase participant program management capabilities, and enhance the effectiveness of communication and stakeholder engagement activities.
To investigate the root causes of the problem, a number of diagnostic activities were undertaken, including process mapping, audits, interviews and literature reviews. Solution generation workshops with key stakeholders identified and prioritised five key solutions for further development.
- An enrolment checklist to guide enrolment processes
- A roadshow event to engage new sites and increase awareness of the program
- A toolkit document for detailed program implementation advice
- A mentoring program to enhance collaboration and develop peer relationships
- A capability development program to increase participant ability and skills
These solutions are being developed and implemented incrementally from September 2018 through to September 2019. Within this project, each solution has a specified development, implementation and evaluation schedule, designed to align with existing initiative milestones and maximise availability of project resources.
Status
Implementation - The initiative is ready for implementation, is currently being implemented, piloted or tested.
Dates
- Project development: Feb-Mar 2018
- Diagnostic activities: Mar-Jun 2018
- Solution development: Jul-Aug 2018
- Implementation: Sept 2018 – Sept 2019
- Commence evaluation: Nov 2018
- Complete evaluation: Dec 2019
Implementation sites
Agency for Clinical Innovation
Partnerships
Centre for Healthcare Redesign
Evaluation
At the time of publication, solutions are being developed and implemented and evaluation of each solution will be undertaken in 2019.
Measures to be assessed include:
- median time taken to enrol in NSQIP
- proportion of participant sites with quality improvement plans endorsed by authorising sponsors
- proportion of quality improvement initiatives sustained for one year or more.
Lessons learnt
- Comprehensive understanding of root cause is critical to the development of appropriate solutions - ensure that sufficient resources are dedicated to diagnostic activities.
- This project focused on the development of solutions applicable to all NSW Health districts. As such, broad representation on working parties was essential.
- Similarly, comprehensive testing of proposed solutions before implementation was crucial to ensure acceptability to the broad target audience.
References
- Cohen ME, et al. Improved Surgical Outcomes for ACS NSQIP Hospitals Over Time: Evaluation of Hospital Cohorts With up to 8 Years of Participation. Annals of Surgery. 2016;267-273.
- Montroy J, et al. Change in Adverse Events After Enrollment in the National Surgical Quality Improvement Program: A Systematic Review and Meta-Analysis. PLoS One. 2016:11.
- Ko CY, et al. The American College of Surgeons National Surgical Quality Improvement Program: achieving better and safer surgery. Joint Commission Journal on Quality and Patient Safety. 2015:41.
Further reading
ACI. National Surgical Quality Improvement Program
- American College of Surgeons. ACS National Surgical Quality Improvement Program
Contact
Crystal Burgess
Surgical Services Taskforce Manager
Agency for Clinical Innovation
Phone: 0410 550 359
crystal.burgess@health.nsw.gov.au